SciBase Journals
SciBase Cardiology
ISSN 2996-4547
- Article Type: Case Report
- Volume 1, Issue 1
- Received: Nov 20, 2023
- Accepted: Dec 22, 2023
- Published Online: Dec 29, 2023
Multiple Malignant Pericardial Mesothelioma Presenting with Massive Hemorrhagic Pericardial Effusion Diagnosed by PET-CT and Pathological Tests: A Case Report
Lei Huang; Jiacheng Rong*
Cardiovascular Department, Ningbo Hangzhou Bay Hospital, Qianwan New Area, Ningbo, Zhejiang, China.
*Corresponding Author: Jiacheng Rong
Email: jiachengrong@sjtu.edu.cn
Abstract
A 53-year-old female was presented to the emergency department with a 5-day history of chest distress and anhelation, who was a worker in a textile factory with a clear long-time exposure of asbestos for nearly 20 years. Both CT and ultrasound imaging showed the bilateral thoracic effusion and massive pericardial effusion. Besides, following PET-CT (positron emission tomography-computed tomography) indicated several abnormally enhanced lesions on her pericardium, which were considered be be some notable results. Later, the cytopathological and immunohistochemical tests delivered by Pathology Department of Ningbo Hwa Mei Hospital both reported convincing results which supported the ultimate diagnosis of “Multiple Idiopathic Malignant pericardial mesothelioma. Then the immuno-therapy and chemo-therapy were delivered. At first, clinical symptoms soon improved. In the next six months, though chemo-therapy sustained, the patient’s condition kept aggravating. Finally, she passed away approximately six months after she was officially diagnosed.
Keywords: Chest; Immuno-therapy; Chemo-therapy.
Citation: Huang L, Rong J. Multiple Malignant Pericardial Mesothelioma Presenting with Massive Hemorrhagic Pericardial Effusion Diagnosed by PET-CT and Pathological Tests: A Case Report. SciBase Cardiol. 2023; 1(1): 1005.
Case report
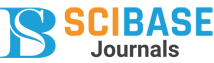
We reported a 53-year-old female presented to the emergency department with a 5-day history of chest distress and anhelation, who had a long-time exposure of asbestos. Her vital sign was as fellows: T 36.8OC, R 20 times/min, P 100 bpm, BP 106/57 mmhg, separately. When later being treated in Emergency Department, a follow-up chest computed tomography (CT) indicated to some special image findings, mainly including the excessive pericardial effusion and the imaging manifestation of mid-ranged pulmonary congestion which was considered to be caused by cardiac systolic limitation (Figure 1). Also, the thoracic B-ultrasound supported part of the imaging from chest CT. And she was initially diagnosed “Hydropericardium with unknown reason”.
Futher clinical findings: As the symptoms of chest distress and anhelation gradually grew apparent, on the examination she was discovered bilateral cardiac enlargement, with two lower limbs found slight depressed edema. The Emergency Department undertook the operation of “left thoracic close drainage”. The liquid released was nearly all hemorrhagic pericardial effusion, of which the total amount reached 600 ml. After the operation, the symptoms above soon miligated, and the edema disappeared. Then liquid biochemical test reported: Total Protein 56.7 g/L, CRP 20.41 mg/L. And the liquid routine examination reported:
1. Appearance: Hemorrhagic and turbid;
2. Cell counting: 1280/ul;
3. Rivalta test: Positive.
Then for further diagnosis and treatment, the patient was immediately hospitalized in the respiratory department and temporarily diagnosed as “Hydropericardium: Tumor? Inflammation? Tuberculosis?”.
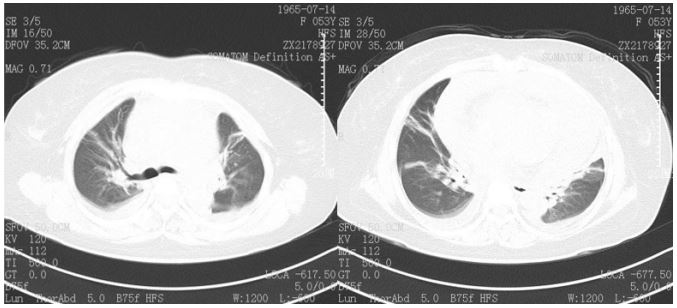
Up to the admission of hospitalization, the result of pet-ct (positron emission tomography-computed tomography) given in emergency department hadn’t been reported yet. TCT (Fluid Based Thin-Layer Cytological Test) and needle aspiration cytological test were performed at once after the admission in Ningbo Hwamei Hospital. On the second day of hospitalization, the result of pet-ct reported and mainly indicated to “Pericardial Tumor (Multiple Idiopathic Mesothelioma)?” (Figure 2).
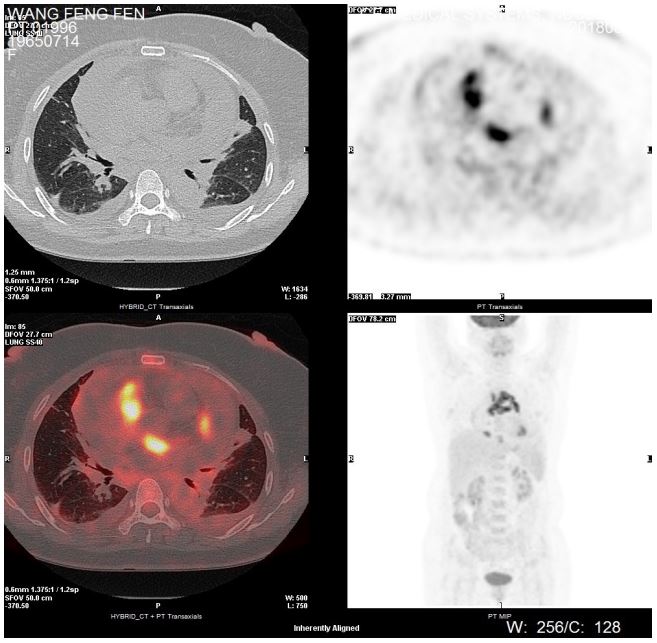
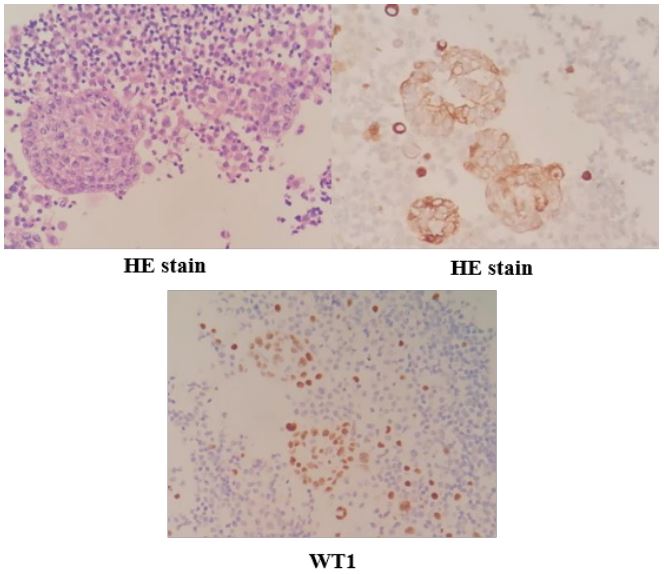
The following immunohistochemical analysis was applied to further estimate it. Three days later, the TCT reported: Multiple masses of malignant cells were found in the smear (Figure 3).
After one week, the effusion immunohistochemical analysis reported: Calretinin (+), Wilms Tumor (+), TTF-1 (-), Napsin A (-), CK5/6 (+), MC (HBME1), (-), CK7 (+), CK20 (-), Villin (-), PAX-8 (-), ER (-) PR (-) (Figure 4). This result further proved its nature and high malignancy. Then the final diagnosis was made: Primary malignant pericardial mesothelioma (PMPM).
Therapeutic intervention: During the period of hospitalization, the pericardial effusion was continuously discharged. The highest volume of daily drainage had reached 1000 ml/24 h. As soon as the final diagnosis was made, the “Recombinant human endostatin” was immediately injected into her pericardial cavity that day. Also the chemo-therapy was given for the first time, of which the combination was “pemetrexed 0.8 g d1 + Nedaplatin 60 mg d1-2”. The ultrasound of next three days showed effusion was no more produced. And main symptoms improved. Thus, the patient was temporarily back home.
Follow‑up and outcome: In the next few months, the patient received chemo-therapy with the same combination for totally four times, whereas chest distress relapsed again one month and half after the fifth chemo-therapy. Compared to CT imaging of the very beginning, new subcutaneous nodules were found in abdominal walls which was considered the metastasis.
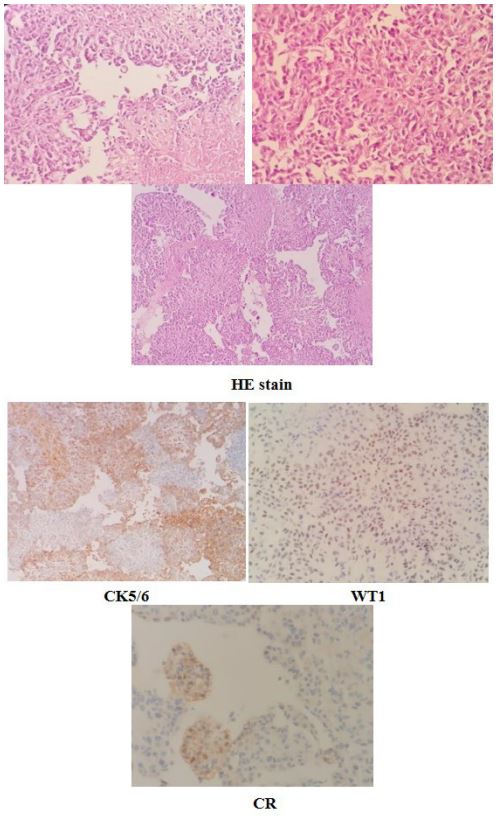
Since then, the patient’s condition rapidly deteriorated. And this situation repeated for several times in the next month. Within this process, the cytopathological test of effusion from left thoracic cavity showed: (Pleural fluid cell mass) malignant cells were found, which was considered the malignant mesothelioma combined with her medical history and immunohistochemistry analysis. The latter reported: Calretinin (-), Wilm’s tumor (+), TTF-1 (-), NapsinA (-), CEA (-), CK5/6 (+), P40 (-), MC (HBME1) (-) (Figure 5). In the following period, though sustaining to be given the positive symptomatic supportive treatment, she eventually died five days later.
Discussion
PMPM seldom emerges. In a large autopsy study, the prevalence of this disorder has been proved to be no more than 0.0022% [1], which is not easy to diagnose at all. As a matter of fact, the PMPM patients have often firstly been referred as pericarditis and cardiac tamponade. Generally speaking, the most common signs and symptoms of PMPM are related to constriction of the heart by the tumour and/or effusion. The latter one is usually discovered as a hemorrhagic effusion [2]. A possible relationship between asbestos exposure and primary pericardial malignancy has been suggested in some studies, but an absolutely definite correlation has not yet been constructed [1]. In addition, it has been reported that PPM is more prevalent in human males and can occur at any age, but is predominantly diagnosed between 50 and 70 years old with a median age of 46 years [3], and here we can see the occurrence in the same age-ranged female group. In addition, it is widely known that PPM is a highly lethal and metastatic disease due to late presentation and poor response to therapy [4]. Although our case points to a quite classical presentation of PMPM which answers low sensitivity to the therapy, it provides an innovative train of thought in diagnosing this rare mortal malignancy which help the patient to be diagnosed at her first hospitalization. During the whole procedure, PMPM follows its conventional occurrence, development and outcome, however, this disease still took some time for doctors to figure it out. In the process of diagnosing, the history of exposing to asbestos, massive hemorrhagic pericardial effusion, cardiac tamponade, pulmonary congestion, heart failure strongly indicate to the possible existence of pericardial malignancy [1,3,5], but our examinations in the early period didn’t show any specificity at all. In this case, we applied pet-ct and pathological examinations at the very beginning, which assisted us to rapidly make the final diagnosis in the early stage accurately. Especially the pet-ct test, it helped us orient the focus in the early stage, which provided the tremendous educational significance in the case of massive pericardial effusion with unknown reason. Without pet-ct, probably we could not be so clear with the direction of subsequent medical treatment quickly. The follow-up recurrence, metastasis and soon death within half a year, which are also very attached to its typical characteristics, further deliver the evidence to our initial judgement. Thus, maybe these two tests can be the gold combination to be included in the diagnostic criteria of PMPM especially for the early diagnosis. To sum up, if patients can afford, we are supposed to offer them choices like pet-ct accompanied with cytology test (add immunohistochemistry analysis in time if necessary) to diagnose PMPM as early as possible, which may help us save more lives.
References
- Suman S, Schofield P, Large S. Primary pericardial mesothelioma presenting as pericardial constriction: a case report. Heart. 2004; 90(1): e4. doi:10.1136/heart.90.1.e4.
- Taguchi S. Comprehensive review of the epidemiology and treatments for malignant adult cardiac tumors. Gen Thorac Cardiovasc Surg. 2018; 66(5): 257-262. doi:10.1007/s11748-018- 0912-3.
- Tajjiou M, Wild W, Sayed N, Flauaus A, Divo M, Schwarzbach M. Primary Pericardial Mesothelioma, Which Was Veiled by a Pleural Empyema: A Case Report and Review. Case Rep Surg. 2019; 2019: 2896810. Published 2019 Sep 11. doi:10.1155/2019/2896810.
- Savarrakhsh A, Vakilpour A, Davani SZ, et al. Malignant primary pericardial mesothelioma presenting as effusive constrictive pericarditis: a case report study. J Cardiothorac Surg. 2021; 16(1): 298. Published 2021 Oct 13. doi:10.1186/s13019-021- 01684-8.
- Godar M, Liu J, Zhang P, Xia Y, Yuan Q. Primary pericardial mesothelioma: a rare entity. Case Rep Oncol Med. 2013; 2013: 283601. doi:10.1155/2013/283601.