SciBase Journals
SciBase Clinical and Medical Case Reports
ISSN 2691-7785
- Article Type: Case Report
- Volume 1, Issue 1
- Received: Sep 25, 2023
- Accepted: Oct 12, 2023
- Published Online: Oct 19, 2023
Successful Thoracoscopic Excision of Left Middle Mediastinal Teratoma in a Girl
Zaparackaite I1 ; Swamy KB2 ; Govani DR3 ; Patel RR3 ; Midha PK4 ; Patel RV3*
1Department of Pediatrics Surgery, Emergency’s Children’s Surgical Hospital, Entebbe, Uganda and the Evelina Children’s Hospital, London.
2Lincoln University College, 2, Jalan Stadium, SS7/15 SS7. 47301 Petaling Jaya, Selangor, Malaysia.
3Department of Pediatrics and Pediatric Surgery, Postgraduate Institute of Child Health & Research and KT Children Govt University Teaching Hospital, Rajkot 360001, Gujarat, India
4J. Watumull Global Hospital & Research Centre, Delwara Road, Mount Abu, Rajasthan 307501, India Affiliated to Medical Faculty of God Fatherly Spiritual University, Mount Abu, Rajasthan.
*Corresponding Author: Ramnik Patel
Department of Pediatrics and Pediatric Surgery, Postgraduate Institute of Child Health & Research and KT Children Govt University Teaching Hospital, Rajkot 360001, Gujarat, India.
Tel: 00447956896641 & Fax: 00441162893395;
Email: ramnik@doctors.org.uk
Abstract
We wish to present a very unusual case of a toddler girl who presented with acute abdomen and features of peritonitis. Inflammatory markers were high but tumor markers were all within normal limits. The plain abdominal radiograph indicated suspicious small free air under the dome of diaphragm. Chest radiograph in standing position confirmed the suspicion but incidentally showed a well-defined soft tissue mass in the mediastinum over left hilar region. Contrast enhanced computed tomography of chest, abdomen and pelvis confirmed mature left mediastinal teratoma and appendicular abscess. The patient underwent laparoscopic drainage of appendicular abscess and appendicectomy and was discharged home after 6 days. An elective thoracoscopic resection of left mediastinal teratoma was performed uneventfully. The patient is asymptomatic with normal tumor markers and chest radiograph at 10 years follow up.
Keywords: Acute abdomen; Appendicitis; Laparoscopy; Mature teratoma; Mediastinal; Thoracoscopy.
Citation: Zaparackaite I, Swamy KB, Govani DR, Patel RR, Patel RV, et al. Successful Thoracoscopic Excision of Left Middle Mediastinal Teratoma in a Girl. SciBase Clin Med Case Rep. 2023; 1(1): 1004.
Introduction
It is a well-known fact that chest pathology may mimic abdominal pathology in emergency and visa versa but it is rare to find a congenital chest pathology as an incidental finding during investigation of acute abdomen in a toddler [1,2]. Mature Mediastinal Teratomas (MMT) are rare congenital tumors with many surgical approaches we wish to present a unique incidentally detected case of mature mediastinal teratoma in a toddler girl who presented with acute appendicular abscess in emergency and during the investigations it was found and successfully resected thoracoscopically.
Case presentation
A 5-year-old girl presented with acute abdominal symptoms of vomiting, diarrhea, abdominal pain and distention, fever and constitutional symptoms of being generally unwell for the duration of last 7 days.
Physical examination showed abnormal vital signs such as pulse 124/min, respiratory rate 26/min, temperature 38.7°C, Patient was listless, had moderate dehydration and was very pale. Abdominal examination showed generalised distention with tenderness and rigidity mainly on the right side of the abdomen and vague lumpish feeling in the right lower quadrant.
Laboratory investigations showed hemoglobin 8.6 Gm%, white cell count 26500x109 /L, polymorphs >90%, CRP of 266 gm/dl. Tumor markers, done later on, including alpha fetoprotein and beta HCG were within normal limits.
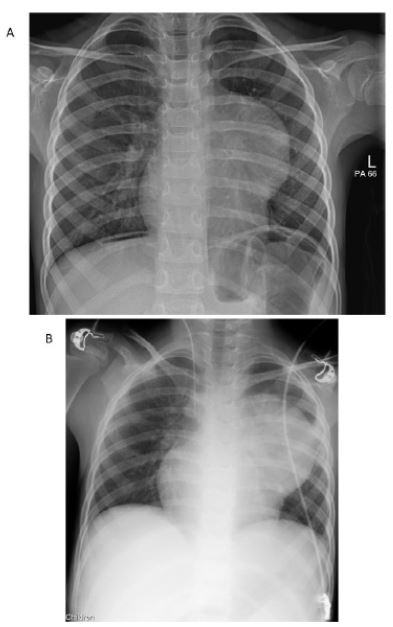
An abdominal radiograph showed generalised bowel distention and ileus with free gas under the diaphragm. Chest radiograph in standing position confirmed some free subdiaphragmatic air below the right hemidiaphragm which showed complete resolution on post-operative radiograph and further abnormal locule of air was seen projected over the liver, and an incidental finding of a large well defined left perihilar mediastinal soft tissue mass (Figure 1A and B).
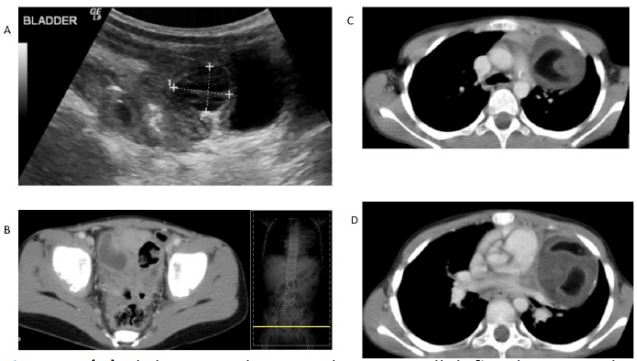
Trans-abdominal ultrasound revealed the presence of a complex mass just above the bladder containing fluid elements with surrounding thick-walled bowel and with small right iliac fossa collection around an appendicular fecalith suggestive of appendicular abscess (Figure 2A).
An oral and intravenous Contrast Enhanced Computed Tomography (CECT) of Chest, Abdomen and Pelvis (CAP) was carried out. CT abdomen and pelvis demonstrated perforated appendix with appendicular calculus and small rim enhancing fluid collections within the abdomen consistent with appendicular abscess (Figure 2B). CT chest showed a large left sided mediastinal mass measuring 5.8x4.7x7.0 cm (AP x transverse x craniocaudal), containing predominantly fluid and fat density with a fleck of mural calcification with some compression of the left main pulmonary artery suggestive of mature mediastinal teratoma (clear borders, size less than 10 cm, mural calcification, mixed contents) (Figure 2C and D).
The patient underwent laparoscopic drainage of appendicular abscess and appendicectomy uneventfully and was discharged home on 6th post-operative day. The need for resection of asymptomatic incidental mature mediastinal teratoma was explained to parents and were happy to undergo thoracoscopically based on their experience with laparoscopic surgery for appendicular pathology in emergency with excellent cosmetic and functional results with quick and complete recovery.
The patent underwent an elective thoracoscopic resection of left mediastinal mature teratoma under general anesthesia with double-lumen intubation and CO2 insufflation of 5-10 mmHg in semi-lateral decubitus position with the surgeon stood behind the patient using Karl-Storz endoscopic instruments to set up trocars using triangle target principle successfully. The fluid component was aspirated to reduce the size of the tumor and facilitate the dissection from the surrounding structures and keep vital neurovascular and bronchopulmonary tissues away to avoid any injury. Dissection and complete removal of tumor was performed with an electrocautery, harmonic scalpel, ligasure or silver clip for hemostasis. The tumor was taken out of the chest by putting into a plastic bag, through a 3 cm skin incision extended from a trocar hole.
Chest drain removed after 48 hours. The post-operative period was uneventful and patient was discharged home on 3rd post-operative day. Histopathological examination showed well defined mature teratoma with predominant skin appendages, nerves, fibrofatty tissue, calcifications, respiratory epithelium and clear resection margins. The patient is asymptomatic and doing well with tumour markers within normal limits and chest radiograph are normal at 10 years follow up.
Discussion
It is a very rare situation to have dual pathology of two varieties such as an incidental congenital mediastinal teratoma in a toddler girl presenting with acute abdomen secondary to an infective pathology. Sacrococcygeal teratoma is the most common teratoma in infants and children and is rare at other locations [3-7]. Extra-gonadal teratomas of the mediastinum are very rare tumors that occur most frequently in the anterior mediastinum. Mediastinal mature teratomas are rare, accounts for 5-10% of all mediastinal tumors.
The incidence is equal for both sexes with a preference for right sided lesions 3 to 4 times higher and most lesions are detected in adolescent or adults. One fourth of all cases are detected incidentally on chest radiograph or a CT scan. The most common symptoms in the mature teratoma group included chest pain (81%), chest tightness or discomfort (52.4%), cough (19.1%), and fever (9.5%) [8].
There are variety of surgical approaches including midline sternotomy, open thoracotomy, minithoracotomy, Video-Assisted Thoracoscopic Surgery (VATS), closed thoracoscopy, or robotic-assisted thoracoscopic surgery. The selection of surgical approach is based on site, size, adhesions and tumor characteristics such as mature/immature/malignant. Currently, the surgical approach has shifted from invasive approaches such as a sternotomy to minimally invasive ones utilizing lung isolation ventilation [7-9].
However, risk factors such as left sided tumor, large tumors, intra-operative tumor adhesion or bleeding, immature or malignant tumour, strong tumor cell adhesion with high grades of adhesion, non-availability of equipment and supportive devices, and less thoracoscopic experience of the surgical team may require conversion, mini-thoracotomy or open thoracotomy which would lead to safety procedures and complete removal of the teratoma. Pre-operative or intraoperative aspiration of fluid contents may be helpful for patients with large mature cystic teratomas to do cytopathological studies and to facilitate thoracoscopic surgery [7,8].
The most MMT are benign, slow growing and have low malignant potential, however, even an incidentally detected MMT needs surgical resection and earlier is better with smaller size of the teratoma so that it can be dealt with minimal invasive surgery. Untreated MMT can lead to continued expansion and pressure effects to the surrounding vital structures, infection, bleeding, rupture, more operative time and morbidity and malignant conversion with increased mortality [10]. If the resection is complete without any complications, prognosis is excellent and long-term prognosis is usually very good without any recurrence or other long term morbidity.
Conclusion
In conclusion, we believe that it may be possible to detect such lesions prenatally or during screening thereafter at an early stage so that smaller size teratomas can be easily dealt with minimal invasive surgery. The thoracoscopic surgery for a mediastinal mature teratoma is feasible, safe and effective with less invasive, less blood transfusion required, less post-operative pain, small invisible scars, less chest drainage duration and hospital stay and wound infection. Left middle mediastinum has less space due to heart, takes longer operative time and is having lots of important nerves-phrenic and recurrent laryngeal as well as perihilar vital structures in close proximity that must be protected from any inadvertent injury.
Declarations
Conflict of interest: The authors have no conflict of interest to declare. No funding source was involved in this study.
Ethical approval: All procedures performed on human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from the parents and all the relatives involved prior to all the procedures. Parents and all involved parties were informed about the procedure.
References
- Trambadia RA, Anthony FM, Chhaniara RA, Patel RV: Left basilar pneumonia simulating perforated appendicitis with peritonitis in a child. J Indian Med Assoc 2023; 121(3): 17-19.
- Govani DR, Scott V, Kumar H, Patel RR, Patel RV and Vaghela SV. “Pus Somewhere, Pus Nowhere Else, Pus above the Diaphragm”- Pediatric Pericarditis Puzzling Professionals. Austin J Clin Case Rep. id1030. 2014; 1: 1-4.
- Patel RV, Marshall D, Gannon C. Paediatric benign cystic monodermal testicular teratoma. BMJ Case Rep. 2014; 2014: pii: bcr2013-202988.
- Patel RV, McNamara V, Jackson P, Drake D: Cervical teratoma simulating thyroglossal cyst. BMJ Case Reports 14 Aug 2013; doi:10.1136/bcr-2013-200671.
- Sinha CK, Anbarasan R, Patel RV, Joshi A, Cherian A. Auto-amputated Ovarian Cysts in Infants: Current Status. JIMA (in pressManuscript ID- JIMA1111629).
- Patel RV, Govani D, Qazi A, Haider N. Dermoid cyst of the glans penis in a toddler. BMJ Case Reports 16 May 2014, 2014; doi:10.1136/bcr-2014-204585.
- Patel RV, Evans K, Sau I, Huddart S. Paediatric giant cervicomediastinal thymolipoma. BMJ Case Reports 20 May 2014, 2014; doi:10.1136/bcr-2014-203585.
- Pham LH, Trinh DK, Nguyen AV, et al. Thoracoscopic surgery approach to mediastinal mature teratomas: a single-center experience. J Cardiothorac Surg. 2020; 15: 35.
- Pham LH, Trinh DK, Nguyen AV, et al. Thoracoscopic surgery approach to mediastinal mature teratomas: a single-center experience. J Cardiothorac Surg. 2020; 15: 35.
- Matsuoka H, Matsubara H, Sugimura A, Uchida T, Ichihara T, et al. Mediastinal mature teratoma perforating the right lung that was successfully resected with complete thoracoscopic surgery: A case report. International Journal of Surgery Case Reports. 2018; 53: 299-302.