SciBase Journals
SciBase Clinical and Medical Case Reports
ISSN 2691-7785
- Article Type: Case Series
- Volume 1, Issue 1
- Received: Sep 23, 2023
- Accepted: Oct 13, 2023
- Published Online: Oct 20, 2023
Maxillary Rehabilitation using the All-on-Four Technique and Computer-Guided Surgery: A Case Report
Mhd Ayham Darwich1 ; Asmaa Alammar2 ; Khaldoun Darwich2 ; Hasan Mhd Nazha3*
1Department of Biomechanics, Faculty of Biomedical Engineering, Al-Andalus University for Medical Sciences, Tartous, Syria.
2Department of Maxillofacial Surgery, Faculty of Dentistry, Damascus University, Damascus, Syria.
3Chair of Computational Mechanics, Faculty of Mechanical Engineering, Otto Von Guericke University Magdeburg, Universitätsplatz 2, 39106 Magdeburg, Germany.
*Corresponding Author: Hasan Mhd Nazha
Chair of Computational Mechanics, Faculty of Mechanical Engineering, Otto Von Guericke University Magdeburg, Universitätsplatz 2, 39106 Magdeburg, Germany.
Email: hasan.nazha@ovgu.de
Abstract
The aim of this study was to evaluate the clinical and radiographic outcomes of the All-on-4 technique in fully edentu-lous maxilla using R2GATE software for flapless, computer-guided surgery and immediate loading. Ten adult patients with fully edentulous maxilla, aged between 35 and 60 years, were included in the study between April 2021 and April 2022. The surgical procedure was performed under local anesthesia and followed the All-on-4 approach with immediate loading of implants using a screw-retained provisional acrylic resin prosthesis on the same day. Final prosthesis was de-livered four months after the surgery. Clinical and radiographic outcomes were evaluated at four- and twelve-months post-operation. The study reported a 95% implant survival rate using the All-on-4 technique. The mean marginal bone level was recorded at 0.35 mm and 0.66 mm during the 4 and 12-month follow-up periods, respectively. Fixed provi-sional prosthesis fracture, abutment, and prosthesis screw loosening were the most frequent mechanical complications reported. Within the limitations of this study, the use of computer-guided surgery in the All-on-4 technique seemed to be a promising treatment option with high implant survival rates that may help reduce post-surgical discomfort and me-chanical complications in the rehabilitation of the edentulous maxilla.
Keywords: Rehabilitation; Tooth loss; Surgery; Computer-assisted.
Citation: Darwich A, Alammar A, Darwich K, Nazha H. Maxillary Rehabilitation using the All-on-Four Technique and ComputerGuided Surgery: A Case Report. SciBase Clin Med Case Rep. 2023; 1(1): 1005
Introduction
Edentulous jaw rehabilitation in elderly patients represents a clinical challenge, especially in the placement of implants [1,2]. The difficulty of rehabilitation depends on bone resorption degree after tooth extraction, the presence of alveolar bone [3], biological and mechanical success of prosthesis, and the patient’s esthetic requirements [4]. Severe alveolar bone resorption requires different surgical techniques for bone augmentation such as external and internal sinus elevation, nerve repositioning, zygomatic implants, and bone grafting [3,5]. Nevertheless, these techniques are most likely rejected by patients because of their cost and post-surgical complications [6,7].
Short implants in the posterior area, tilted distal implants in both “All-on-4”, and “All-on-6” protocols, and distal cantilever are considered alternative treatments for edentulous patients’ rehabilitation [5,8]. The conventional two-stage delayed loading procedure was first suggested by Branemark in 1977 [3,9]. Nowadays, patients’ expectations related to discomfort minimization, ability to immediate loading, and restoration of functional and aesthetical aspects has increased, and this led to the appearance of the one-stage immediate loading procedure [10].
Previous studies reported that immediate loading procedures achieved high survival rates in comparison to conventional delayed loading procedures [8,11]. Moreover, flapless computer-guided surgery is recommended to shorten the healing period and minimize post-operative pain, especially to achieve implant positioning with accuracy [12]. The All-on-4 concept in the maxilla aimed to rehabilitate the edentulous jaw with the achievement of immediate loading [7,8]. This treatment concept involves four implants “two anterior upright implants placed between the lateral incisor and the canine, and two tilted posterior implants placed parallel to the anterior wall of maxillary sinus” [7-10]. There are some advantages of the distal implants’ inclination like better anchoring of implants due to the use of angled longer implants, reduction of cantilever’s length, avoid additional surgical procedures such as sinus elevation and bone grafting [5], and elimination of masticatory stresses applied on the cortical bone around the implants [5,7].
Many of the previous clinical studies with short-term followup periods supported the use of the “All-on-4” technique to rehabilitate the fully edentulous maxilla. The success rate for 5-years follow-up ranged between 91.3-93% for tilted distal implants, and between 95.2-98.9% for axial implants [12,13]. The development of computer technology allowed surgeons to combine between “All-on-4” protocol and 3D design software, which depends on the accuracy of computed tomography images used for model generation and implant localization. Conventional surgical guides were fabricated of acrylic resin, which is an autoclavable, biocompatible resin suitable for 3D printing of surgical guides used in implantology. Material properties mainly vary depending on model geometry, printing orientation, and used sterilization methods [14].
Radiographic imaging plays a significant role in implantology. Furthermore, the introduction of CBCT (cone beam computed tomography) with embedded software facilitated two-dimensional radiographic imaging with a higher spatial resolution compared to CT (computed tomography). High exposure to ionizing radiation is the main disadvantage of CBCT and CT compared to other radiographic techniques. This exposure limits the use of those modalities during short follow-up periods. On another side, MRI (magnetic resonance imaging) is increasingly used in dental diagnostics, as image artifacts were low since MRI does not use ionizing radiation, which may cause biological damage [15].
However, there is a lack of information or understanding about the clinical and radiographic outcomes of the All-on-4 technique in fully edentulous maxilla. The value of performing this study lies in the potential to improve patient outcomes and quality of life by offering an effective and predictable treatment option for the rehabilitation of the edentulous maxilla. It also has the potential to reduce post-surgical discomfort and mechanical complications. Furthermore, this study may contribute to the development of evidence-based guidelines for the use of computer-guided surgery in the All-on-4 approach.
This study aims to evaluate the clinical and radiographic outcomes of the All-on-4 technique in fully edentulous maxilla using R2GATE software for flapless, computer-guided surgery and immediate loading (one-day implant).
Materials and methods
This study included a sample of 10 adult patients with edentulous maxilla, consisting of 8 men and 2 women, who provided informed consent after obtaining ethical approval (number 1933 on 18 March 2021). The patients’ ages ranged from 35 to 60 years and they were all recruited from the faculty of dentistry at Damascus University between April 2021 and April 2022.
Inclusion criteria: Adult patients aged between 35 and 60 years, fully edentulous maxilla; The opposite jaw should be fully edentulous with full removable denture (Attention was taken not to vary the biting force of the patients in order to eliminate results variation related to this factor); Good oral hygiene and periodontal health (normal color of the mucous membrane, no abrasions, no signs of suppuration, infection or formation of fistulas, and sufficient keratinized mucosa); Healthy patients with well-controlled systemic disease, extraction of any remaining dental units had been performed earlier to the surgery by 3 months at least; Good and sufficient quality of the residual bone in the anterior area of the maxilla was determined via CBCT analysis (at least 13 mm of height and 5.5 mm of diameter) allowing the placement of four implants with a diameter of at least 3.75 mm and a length of at least 10 mm; D2 or D3 bone density values (expressed by HU units) obtained by medical CBCT according to Misch 1988 [16], allowing a placement of the implants with an application of insertion moment of 35 N.cm at least.
Exclusion criteria: Smokers; Substance or alcohol abuse; Intake of bisphosphonate medication; Patients with current irradiation of head and neck area or in the last 12 months; Poorly controlled systemic disease (such as uncontrolled diabetes); Psychiatric problems; Pregnant and lactating women; Poor oral hygiene; Active periodontal disease; Sever bruxism; Parafunctional habits; Patients with insufficient mouth opening of less than 40 mm; Insufficient quality and quantity of the residual bone in the anterior area of the maxilla.
Pre-operative procedure
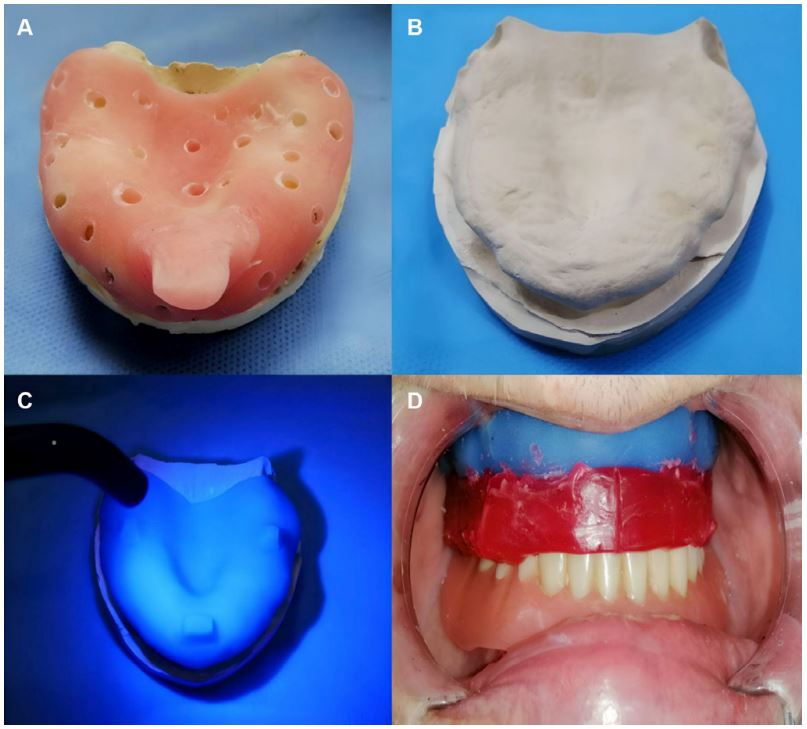
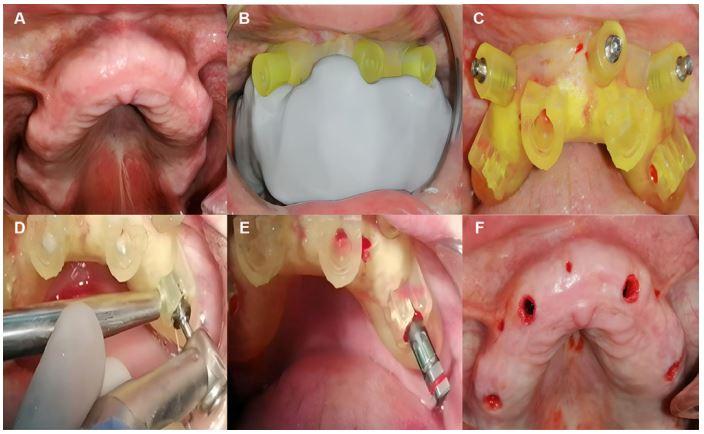
Photographic images of all patients fully smiling were obtained before the surgery for aesthetic and functional evaluation. Firstly, an alginate impression was made to form a primary stone model. An individual tray was fabricated in the laboratory depending on the previous model (Figure 1A). Then, an accurate silicon impression was taken by the individual tray to form the final study model (Figure 1B).
This was checked for distortion or damage, and the outline of the tray base was drawn. All the undercuts of the model were blocked out using paraffin wax. Separating cream or oil was spread on the surface to prevent sticking with tray resin. The performed tray resin was spread on the model and trimmed superfluous parts using a knife. Then, it was cured using a light cure machine, and separated from the model, any sharp edges were trimmed (Figure 1C). After that, the study models were mounted on a mean-value articulator, and a wax rim on a tray base was built to register the relationship between upper and lower jaws. The standard height of the upper rim was 22 mm. A customized resin base was seated in the patient's mouth to adjust the wax rim height and take the centric relation position of the mandible (Figure 1D).
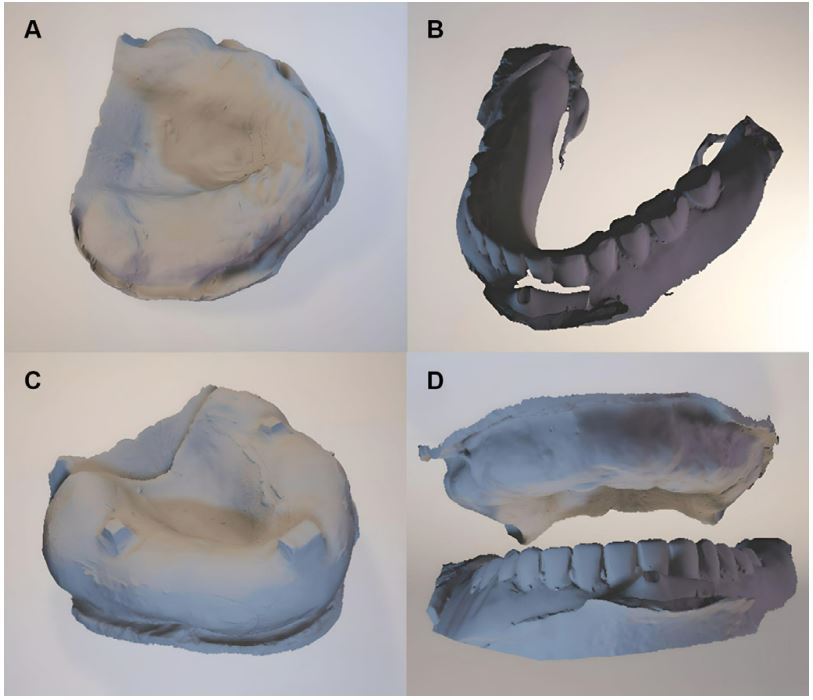
The midline and canine positions were marked on a wax rim and the teeth arrangement was set accordingly. A customized resin base and an opaque radiographic index were also placed in the patient's mouth prior to obtaining Cone Beam Computed Tomography (CBCT) images. The patient's head was fixed with a chin holder during the CBCT scan, while avoiding any contact with the CBCT bite block. The opaque radiographic index served as a reference point for assessing the location and extent of a particular condition or pathology. Afterward, all of the maxilla and mandible stone casts, maxilla resin base, and interocclusal records were scanned using a dental lab scanner (as shown in Figure 2).
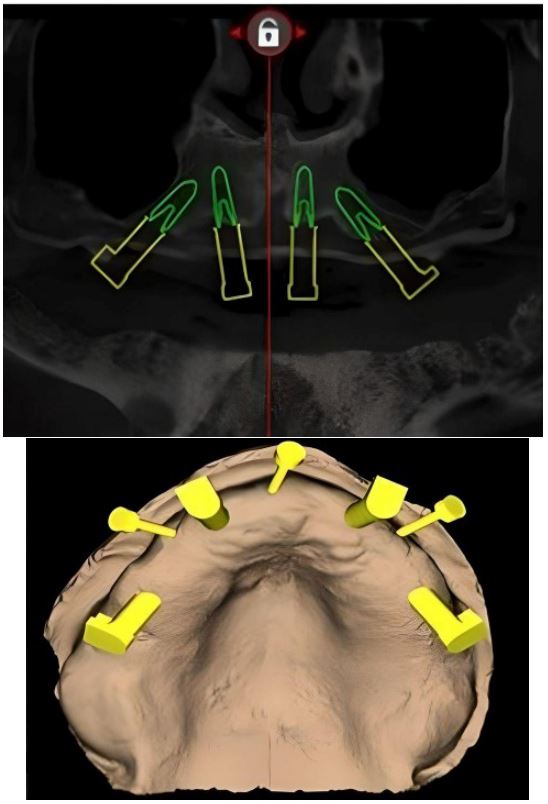
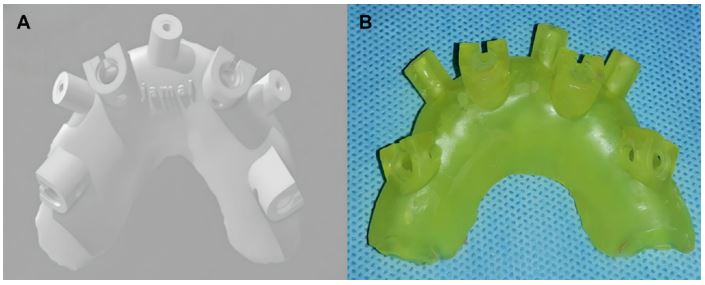
All the previous scan data (STL format) and CBCT data (sliced DICOM) were transferred to a computer for using R2GATE software (Version 3.7.4, R2gate, Co., Ltd., Seoul, South Korea). This allowed the designing of a 3D surgical guide according to the "all-on-4" concept (Figure 3). Then the planning data were sent to a manufacturing lab. At the dental laboratory, a 3D surgical guide was printed by using a 3D dental printer (The UNIZ slash 2 which features LCD stereolithography technology) (Figures 4A and 4B).
As suggested by Puig [1], an hour before surgery all patients received antibiotics (amoxicillin and clavulanic acid 875/125 mg), for patients allergic to penicillin (diacetyl-midecamycin 900 mg) was used, ibuprofen 600 mg to manage post-operative pain, diazepam 5-10 mg for sedation if needed, extra-oral and intra-oral antisepsis was achieved with 2.0% chlorhexidine for 1 min before surgery. Anesthesia was administered using local infiltration (2% lidocaine with 1:100000 epinephrine).
Surgical procedure
A putty surgical index was taken by bite registration between the surgical guide on the maxilla stone cast and the opposite mandible on the articulator. This permitted the correct placement of the surgical guide and putty bite together in the patient's mouth. Patients were then asked to make a maximum biting with maximum occlusal force to prevent any movement (Figure 5A). After that, the guide was stabilized with three screw anchor pins placed in triangular form, which is highly recommended to achieve a better fixation using a hand screwdriver (2Ø x13 mm) (Figure 5B).
The flapless implant surgery was achieved by using the "All-on-four" concept. Two axially orientated implants were positioned in the region between the lateral incisor and canine, and two tilted distal implants were placed parallel to the anterior wall of the maxillary sinus. Implants lengths ranged from 10 to 15 mm, and diameters were 3.75 to 5.5 mm with an application of insertion moment of 35 N.cm allowing an immediate loading. Surgical drilling was performed as instructed by the manufacturing company (MegaGen, Alnajah company, R2GATE protocol) (Figure 5C).
R2GATE drilling protocol
All drills consist of a drill, drill guide, and drill stopper as one body, and no need for metal sleeves or spoons. The initial drill was used to mark the drilling start-point on bone; the second drill also removes excess bone above the fixture platform for a better connection with the prosthesis. Graduated drilling was then used to increase depth and diameter. The drilling has not been started until the drilling guide is completely inserted into the guide hole, and always start drilling at low RPM (300-500 RPM) with up and down drilling motions to increase osteotomy depth in 1 mm increments. R2GATE software (Version 3.7.4, R2gate, Co., Ltd., Seoul, South Korea) offers a color-coded analysis of bone morphology which identify the invisible bony structure for predicting optimal drilling sequence to achieve strong initial stability (recommended drilling speed 500-800 RPM). Consequently, the implants were inserted via the R2 Guide using an implant carrier. Concerning fixture depth control, the upper line of the implant carrier was aligned with the R2 Guide window, and align green was also aligned with the R2 Guide window turning in the buccal direction to hex position control (Figure 5D). Finally, anchor pins were loosed and the R2 Guide was removed from the patient's mouth (Figure 5E). The initial stability of the four implants was measured by using ISQ device. The measurements were taken in both directions (misodistal and Bucco-palatal) and repeated twice in every direction. The mean of the four measurements of each implant has been calculated. It should be ≥65 N.cm for immediate loading [17].
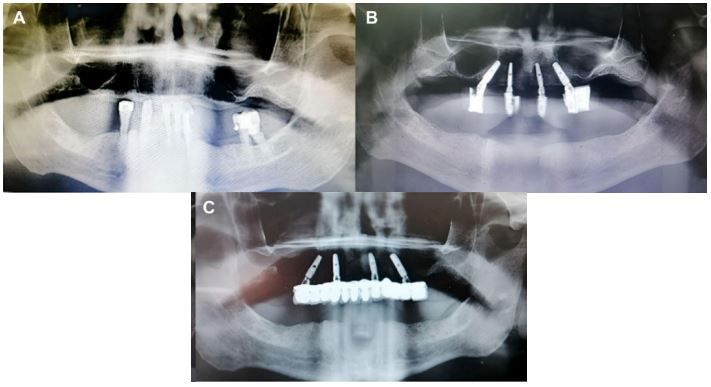
Once implants were placed, multi-unit abutments could be placed 30° multi-unit abutment in posterior/tilted implants and straight or 17° multi-unit abutments in the anterior by using a multi-unit holder to be parallel together, and tightened to 15 N.cm (Figure 6A). The position of multi-unit abutments has been indexed on the intaglio surface of the patient's removal denture and hollowed-out space in the denture for temporary coping multi-unit. This latter was attached to multi-unit abutments and placed hollowed-out dentures over temporary coping multi-unit cylinders (passive fit). After that, the over-height of temporary coping multi-unit has been reduced to allow the patient to bite down.
Light curing flow composite was used to pick up temporary coping cylinders with a provisional denture, then unscrewed and removed the prosthesis with temporary coping multiunit cylinders. Then, any sharp angles or edges on the intaglio surface of the denture have been removed (Figures 6B and 6C). A provisional screw-retained implant denture was attached with torque to 15 N.cm and filled in the screw hollow with flow composite. Finally, by using articulation paper, the occlusion was adjusted, and reducing any high spots to level occlusion (Figures 6D and 6E). Post-operative prescription [17,18]: Nonsteroidal anti-inflammatory drugs (Ibuprofen 600 mg / 4 times daily for 3 days); Oral antibiotics prophylaxis (Amoxicillin 500 mg / 3 times daily for 7 days); Analgesic (Paracetamol 750 mg if needed); 0.12% chlorhexidine rinse (2 times for 1 minute during 2 weeks).
Post-operative instructions
Soft food diet is recommended within 4 months postoperative while the osseointegration of implants is happening; Good oral hygiene: For the first 14 days, post-operatively the patients should use chlorhexidine rinse, after 2 weeks use water pick and soft bristle toothbrush with non-abrasive toothpaste; Recall hygiene visits are recommended every week in the first month postoperatively, then every 3 months to evaluate prosthesis, implants, and tissue healthy.
After a healing period of 4 months, post-operatively a final prosthetic rehabilitation could be started as follows (Figures 7 and 8): Unscrew the provisional denture; Attach open tray multi-unit impression-transfer to multi-unit abutments; Lute the impression transfers together with metal wire to ensure accuracy; Make sure the tray clears the open tray impression transfers; Take the open tray impression by using light and heavy body impression materials; The final titanium prosthetic framework was made and included 12 teeth with a maximum of the one-unit cantilever from aesthetic resin material; The final prosthesis should seat firmly against the soft tissue, and be retained by screws with a moment of 15 N.cm; Block out screw hollows with acrylic or flow composite.
Follow up assessment measures
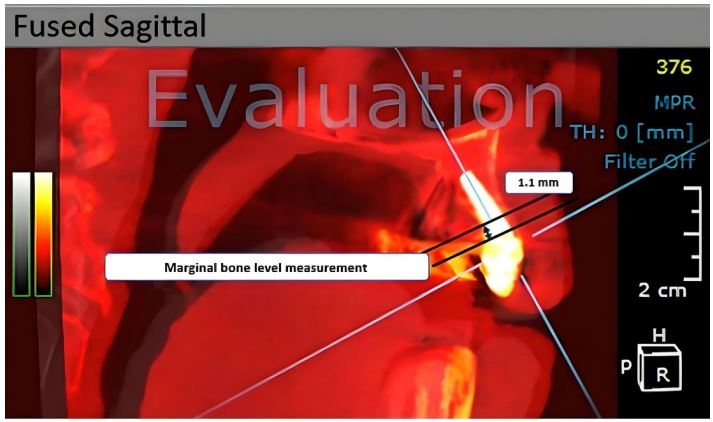
OnDemand3D software (Version 1.0.0.94, Cybermed, Seoul, South Korea) was used to assess the peri-implant bone resorption at intervals of 4- and 12-months following surgery. The operator first selects the implant of interest and defines the measurement area. The software then automatically identifies and marks the alveolar bone crest and implant platform, and calculates the distance between them. The resulting measurement is displayed on the screen and can be saved for further analysis or comparison.
Using CBCT images of maxilla bone, peri-implant resorption was assessed by measuring the distance between the reference point (implant platform: the horizontal interface between the abutment and the implant), and the marginal bone level, which compared with the value registered after surgery by using OnDemand3D software (Figure 9).
Clinical evaluation of the implant survival was calculated at each re-assessment (4- and 12-months follow-up period postoperatively) (Figure 10), plaque index (PI) was evaluated on the mesial, distal, buccal, and palatal surface of the multi-unit abutments at each re-assessment (4 and 12 months).
Probing Depth (PD) was also measured after the prosthesis was removed by using 15 UNC periodontal probes at the same previous surface (mesial, distal, buccal, and palatal) to the nearest millimeter at 4- and 12-months follow-up post-operatively, Bleeding on Probing (BoP) was tested after the removing of prosthesis 4 and 12 months follow up period at the same surfaces as described above. Biological complications (infection, and fistula), and mechanical complications (screw loosening, implant fracture, and fracture of the prosthesis). All the previous clinical registrations were performed by the same-trained examiner.
Statistical analysis
The statistical parameters for this study were determined using G*Power software (Version 3.1.9.7., University of Mannheim, Germany). A confidence level of 95% (α=0.05) and a sampling power of 80% (1-B=0.8) were used to calculate the appropriate sample size, based on the SD values of marginal peri-implant bone resorption in a pilot study sample. Data analysis was performed using SPSS Statistics software (Version 13, IBM Corp., Armonk, USA). Descriptive analysis, Wilcoxon signed ranks test, and T-test were used for statistical analysis, and a Pvalue <0.05 was considered significant.
Results
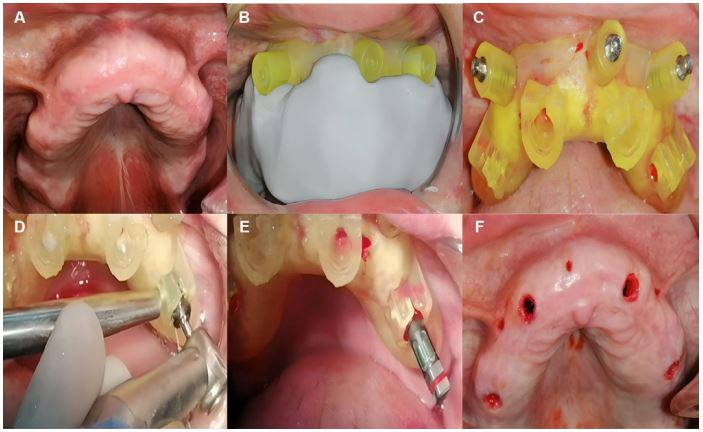
Ten patients (two women and eight men) aged between 35 and 65 years were rehabilitated according to the "All-on-4" concept by using flapless computer-guided surgery. Forty implants were immediately positioned (20 axial implants and 20 tilted implants). The results were as follows:
Two of the 40 implants (one axial implant and one tilted implant) in two patients were lost after two months post-operatively, pointing to an overall survival rate of 95%. In terms of Plaque Index (PI), Probing Depth (PD), and Bleeding on Probing (BoP); all patients showed acceptable oral hygiene during follow-up intervals with a mean PI below 30% after 4 months postoperatively, and below 45% after 12 months without significant differences over time (P< 0.05) (Table 1). This coincides with low BoP levels and a significant time effect (P=0.008) (Table 1). The mean of PD was (3.04 and 2.51) after 4 and 12 months respectively. Moreover, the PD seemed to be reduced after 12 months postoperatively (Table 2). The vast majority of implants showed shallow pockets (≤3 mm).
Table 1: Wilcoxon signed ranks test values for both PI and BoP index.
| The index | Wilcoxon signed ranks test values for both PI and BoP index | ||
|---|---|---|---|
| Calculated z value | P-value | Statistically significant difference | |
| PI | -1.856 | 0.063 | - |
| BoP | -2.646 | 0.008 | + |
Regarding the Marginal bone level, the overall value of the mean marginal bone level after 4 months post-operatively was 0.66 mm and 0.35 mm after 12 months of the follow-up period. A significant decrease in the marginal bone level was observed over time (P=0.040). This result can be explained as follows: During the immediate functional loading period, occlusal forces affect the bone. Before the implantation, the bone seems to become fully mineralized, but with a formation of a low-mineralized mature moving bone, resulting from the excessive pressure related to implant insertion. This also seems to have a role in necrotic bone replacement due to surgical trauma and implant insertion.
After 4 months (period of healing and bone remodeling), the bone turns into primary mineralized lamellar bone (70-85%), and after that, it turns into a secondary mineralized lamellar bone, and this is accompanied by crystals maturation and completion of mineralization after approximately 8 months (15- 30%). Most specifically, the effect of the occlusal force seems to be greater on the moving bone during the first 4 months after implantation, than on the secondary mineralized lamellar bone after 1 year.
No biological complications such as pain or infection have been reported. No aesthetic, phonetic, or chewing ability problems were observed. Two patients showed fractures in their provisional acrylic prostheses during the immediate loading period (healing period). Screw loosening occurred in four implants (one axial implant and three tilted implants). Screw loosening in both fixed and provisional prostheses was observed. No other mechanical complications occurred.
Table 2: T-test values for PD index.
| Follow-up | T-test values for the PD index | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of implants |
Arithmetic mean |
Standard de- viation (mm) |
Standard error |
Minimum value |
Maximum value |
The arithmetic mean difference |
Calculated t value |
P-value |
Statistically signifi- cant difference |
||
| 4 | months | 40 | 3.04 | 0.35 | 0.05 | 1.1 | 3 | -0.18 | -2.034 | 0.049 | + |
| 12 | months | 40 | 2.51 | 0.28 | 0.04 | 0.9 | 2.8 | -0.25 | -2.416 | 0.021 | + |
Discussion
The findings of this study suggest that the rehabilitation of a fully edentulous maxilla using the "All-on-4" concept with flapless computer-guided surgery is promising, with a 95% implant survival rate achieved after 12 months postoperatively. The implant survival rate observed in this study is comparable to the study by Rossi et al. [19], which showed high implant survival rates, with a 95.3% survival rate for zygomatic implants and a 98.8% survival rate for conventional implants. The mean marginal bone loss was 1.27 mm for zygomatic implants and 0.87 mm for conventional implants.
Clinical parameters, such as PI, BoP, and PD, were evaluated in this study, and the majority of implants showed shallow pockets (≤ 3 mm), with PD reducing after 12 months postoperatively. The marginal bone level decreased significantly over time, with a mean value of 0.35 mm after 12 months of follow-up, indicating limited marginal bone loss.
The use of computer-guided implantation for the rehabilitation of a fully edentulous maxilla with the "All-on-4" concept is a promising approach that can shorten the procedure and facilitate the operation of patients and surgeons. The development of 3D imaging has raised expectations in implant dentistry, allowing for precise visualization of skeletal components in the craniofacial region. 3D models can be manipulated in any direction, providing valuable information to the surgeon without the need for patient recall or clinical examinations. The use of 3D digital planning software can aid in simulating treatment outcomes and allowing prosthesis modification.
In comparison to Ferri et al. [20], the complication rate of the suggested protocol was low, with no reported biological complications. The most common complications were mechanical in nature, such as provisional acrylic prosthesis fracture and screw loosening, but were easily resolved by repairing the provisional prosthesis and retightening the abutment and prosthetic screws. The authors also noted a low rate of implant failure, with a 98.6% survival rate for maxillary implants and a 99.4% survival rate for mandibular implants.
Recent studies have shown similar success rates, with a 100% survival rate for both maxillary and mandibular implants. The mean marginal bone loss was 0.53 mm for maxillary implants and 0.36 mm for mandibular implants [21], while another reported a 97.1% implant survival rate after three years of followup [22]. These studies support the use of the "All-on-4" concept and computer-guided surgery as a reliable and effective treatment option for fully edentulous maxilla.
The limitations of this study include the short follow-up period and lack of a control group. Prospective studies are needed to further evaluate the impact of other risk factors, such as smoking and marginal bone loss, in rehabilitated patients according to the "All-on-4" concept using computer-guided surgery.
Conclusion
This study suggests that the "All-on-4" concept, utilizing flapless computer-guided surgery for the rehabilitation of a fully edentulous maxilla with immediate fixed prosthesis placement, can be a highly effective and predictable treatment option with a high survival rate and great patient acceptance. Although flapless computer-guided surgery may require a skilled and experienced surgeon, the potential benefits of this treatment modality make it a promising option for patients seeking full-arch rehabilitation.
Declarations
Author contributions: Conceptualization, A.A. and M.A.D.; methodology, K.D and A.A.; software, visualization; H.M.N.; validation, writing-original draft preparation, A.A.; writing-review and editing, M.A.D and H.M.N.; supervision, project administration; K.D. and M.A.D. All authors have read and agreed to the published version of the manuscript.
Funding: This research received no external funding.
Institutional review board statement: The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee at Damascus University (number 1933 on 18 March 2021).
Informed consent statement: The patients provided an informed consent statement.
Data availability statement: Data are available on request from the corresponding author
Conflicts of interest: The authors declare no conflicts of interest.
References
- Puig C. A Retrospective Study of Edentulous Patients Rehabilitated According to the “all-on-Four” or the “All-on-Six” Immediate Function Concept Using Flapless Computer-Guided Implant Surgery. Eur. J. Oral Im-plantol. 2010; 3: 155-163.
- Habib SH, Gul A, Malik MO, Habib SR, Khalil A. Evaluation of Oral Hygiene and Dietary Status among Eden-tulous, Dentate and Denture Wearers in the Elderly. Khyber Med. Univ. J. 2020.
- Merheb J, Vercruyssen M, Coucke W, Quirynen M. Relationship of Implant Stability and Bone Density Derived from Computerized Tomography Images. Clin. Implant Dent. Relat. Res. 2018; 20: 50-57.
- Maló P, de Araújo Nobre M, Lopes A, Ferro A, Nunes M. The All-on-4 Concept for Full-Arch Rehabilitation of the Edentulous Maxillae: A Longitudinal Study with 5-13 Years of Follow-Up. Clin. Implant Dent. Relat. Res. 2019; 21: 538-549.
- Lopes A, de Araújo Nobre M, Santos D. The Workflow of a New Dynamic Navigation System for the Insertion of Dental Implants in the Rehabilitation of Edentulous Jaws: Report of Two Cases. J. Clin. Med. 2020; 9: 421.
- Cassetta, M, Giansanti, M, Di Mambro, A, Stefanelli, L. Accuracy of Positioning of Implants Inserted Using a Mucosa-Supported Stereolithographic Surgical Guide in the Edentulous Maxilla and Mandible. Int. J. Oral Maxillofac. Implants. 2014; 29: 1071-1078.
- Vercruyssen M, Cox C, Naert I, Jacobs R, Teughels W, et al. Accuracy and Patient-Centered Outcome Variables in Guided Implant Surgery: A RCT Comparing Immediate with Delayed Loading. Clin. Oral Implants Res. 2016; 27: 427-432.
- Reyes A, Turkyilmaz I, Prihoda TJ. Accuracy of Surgical Guides Made from Conventional and a Combination of Digital Scanning and Rapid Prototyping Techniques. J. Prosthet. Dent. 2015; 113: 295-303.
- Peñarrocha-Diago M, Peñarrocha-Diago MA, Zaragozi-Alonso R, Soto-Peñaloza D. M on behalf of the Ticare Consensus Consensus Statements and Clinical Recommendations on Treatment Indications, Surgical Proce-dures, Prosthetic Protocols and Complications Following All-On-4 Standard Treatment. 9th MozoGrau Ticare Conference in Quintanilla, Spain. J. Clin. Exp. Dent. 2017.
- Zhou W, Liu Z, Song L, Kuo CL, Shafer DM. Clinical Factors Affecting the Accuracy of Guided Implant Sur-gery-A Systematic Review and Meta-Analysis. J. Evid. Based. Dent. Pract. 2018; 18: 28-40.
- Saleh Saber F, Ghasemi S, Koodaryan R, Babaloo A, Abolfazli N. The Comparison of Stress Distribution with Different Implant Numbers and Inclination Angles in All-on-Four and Conventional Methods in Maxilla: A Fi-nite Element Analysis. J. Dent. Res. Dent. Clin. Dent. Prospects. 2015; 9: 246-253.
- Liu, T, Mu, Z, Yu, T, Wang, C, Huang, Y. Biomechanical Comparison of Implant Inclinations and Load Times with the All-on-4 Treatment Concept: A Three-Dimensional Finite Element Analysis. Comput. Methods Bio-mech. Biomed. Engin. 2019; 22: 585-594.
- Ferraz CC, Barros RM, Ferraz FC, Mundstock AA, Maior BS. Analysis of Stress Distribution in Ceramic and Titanium Implants in Alveolar Sockets of the Anterior Region of the Maxilla. J. Clin. Exp. Dent. 2019.
- Juneja M, Thakur N, Kumar D, Gupta A, Bajwa B, et al. Accuracy in Dental Surgical Guide Fabrication Using Different 3-D Printing Techniques. Addit. Manuf. 2018; 22: 243-255.
- Reda R, Zanza A, Mazzoni A, Cicconetti A, Testarelli L, et al. An Update of the Possible Applications of Mag-netic Resonance Imaging (MRI) in Dentistry: A Literature Review. J. Imaging. 2021; 7: 75.
- Sogo M, Ikebe K, Yang TC, Wada M, Maeda Y. Assessment of Bone Density in the Posterior Maxilla Based on Hounsfield Units to Enhance the Initial Stability of Implants: Bone Density in Posterior Maxilla by CT Value. Clin. Implant Dent. Relat. Res. 2012; 14: e183-e187.
- Bavetta G, Bavetta G, Randazzo V, Cavataio A, Paderni C, et al. A Retrospective Study on Insertion Torque and Implant Stability Quotient (ISQ) as Stability Parameters for Immediate Loading of Implants in Fresh Ex-traction Sockets. Biomed Res. Int. 2019; 2019: 1-10.
- Spinelli D, DE Vico G, Schiavetti R, Bonino M, Pozzi A, et al. Immediate Loading of Four Implants BTLock® in the Maxilla and Provisional Restoration with Guide-Surgery SimPlant, Materialise®: Case Report. Oral Im-plantol. (Rome). 2010; 3: 10-19.
- Rossi F, Botticelli D, Arcuri L, et al. Zygomatic Implants Placed in Immediate Function through Extra-Maxillary Surgical Technique and 45 to 60 Degrees Angulated Abutments for Full-Arch Rehabilitation of Extremely Atrophic Maxillae: Short-Term Outcome of a Retrospective Cohort. J Clin Med. 2021; 10: 2095.
- Ferri M, Stellini E, Berton F, Bottega S, Siviero M, et al. Clinical Complications and Maintenance Requirements of Immediate Loading Full-Arch Rehabilitation with the All-on-4 Concept: A Retrospective Cohort Study with 1 to 10 Years of Follow-Up. J. Clin. Med. 2021; 10: 1342.
- De Angelis P, Passarelli PC, Gasparro R, D’Amato S, D’Addona A. Immediate Loading of Full-Arch Im-plant-Supported Fixed Prostheses Using Computer-Guided Implant Placement: A Prospective Clinical Study. J. Clin. Med. 2021; 10: 972.
- Alhammadi MS, Al-mashraqi AA, Alnami RH, Ashqar NM, Alamir OH, et al. Accuracy and Reproducibility of Facial Measurements of Digital Photographs and Wrapped Cone Beam Computed Tomography (CBCT) Pho-tographs. Diagnostics (Basel) 2021; 11: 757.