SciBase Journals
SciBase Clinical and Medical Case Reports
ISSN 2691-7785
- Article Type: Case Series
- Volume 1, Issue 2
- Received: Sep 11, 2023
- Accepted: Oct 17, 2023
- Published Online: Oct 24, 2023
Does Adding Percutaneous Fixation to Vertebroplasty Result in Significant Improvement in Clinical Outcomes Compared to Vertebroplasty Only? A Retrospective Series of 51 Cases at a Mean of 3 Years
Abdelrady Mahmoud1 ; Ahmed Nageeb Mahmoud1,2*; Hemil Maniar2 ; Sherif Dabash1,3; Ahmed H. Elhessy4 ; Daniel Scott Horwitz2
1Orthopedic Surgery Department, Ain Shams University Faculty of Medicine, Cairo, Egypt.
2Orthopedic Surgery and Spine Department, Geisinger Medical Center, Danville, Pennsylvania, USA.
3Orthopedic Surgery Department, WVU medicine, Keyser, West Virginia, USA.
4Orthopedic Surgery Department, Nemours Children Health, Jacksonville, Florida, USA.
Investigations were performed at Ain Shams University Hospitals, Cairo, Egypt.
*Corresponding Author: Ahmed Nageeb Mahmoud
Orthopedic Surgery Department, Ain Shams University Faculty of Medicine, Cairo 11566, Egypt.
Geisinger Musculoskeletal Institute, 100 N Academy Ave Danville, PA 17821, USA.
Tel: +15702454062 & +15702140824;
Email: anmahmoud@med.asu.edu.eg & amahmoud@geisinger.edu
Abstract
Background: While vertebroplasty is a well-known technique for management of osteoporotic vertebral fractures, significant incidence of refracture and re-collapse can occur after vertebroplasty, which may necessitate a revision surgery in such weak bone conditions. The aim of this study is to compare the mid-term clinical outcomes of vertebroplasty versus vertebroplasty plus percutaneous fixation for management of osteoporotic vertebral fractures.
Methods: This retrospective study included 51 patients who received surgical treatment for lumbar osteoporotic fractures. Group 1, the Vertebroplasty (VP) group included 28 patients, while group 2, Vertebroplasty Plus Percutaneous Fixation (VPPF) included 23 patients. The outcomes were measured using the Visual Analogue Scale (VAS), Oswestry Disability Index (ODI), clinical and radiological findings for vertebral refracture or re-collapse, along with documenting perioperative and postoperative complications.
Results: After a mean follow up of 36.7 months, the VPPF group had less incidence of mechanical complications, such as refracture, re collapse and cement leakage. On the other hand, the VP group had a lower surgery time, blood loss and wound complications. There were no significant differences in the VAS clinical score at the last follow up, while the VPPF group had slightly better ODI scores.
Conclusions: VPPF resulted in more stable management for osteoporotic vertebral fractures with a less incidence of mechanical complications.
Keywords: Osteoporosis; Vertebral fractures; Vertebroplasty; Percutaneous fixation.
Citation: Mahmoud A, Mahmoud AN, Maniar H, Dabash S, Elhessy AH, et al. Does Adding Percutaneous Fixation to Vertebroplasty Result in Significant Improvement in Clinical Outcomes Compared to Vertebroplasty Only? A Retrospective Series of 51 Cases at a Mean of 3 Years. SciBase Clin Med Case Rep. 2023; 1(2): 1006.
Introduction
Osteoporotic Vertebral Compression Fractures (OVCF) represent a major health problem worldwide due to the aging of population and increased prevalence of osteoporosis [1]. With an incidence reaching about 15% of all vertebral fractures, OVCF affect mainly vertebrae at the thoracolumbar junction [2,3].
While conservative management is usually the initial therapy for OVCF, it does not prevent progression of deformity and adjacent segment fracture due to change of the spinal mechanics [2,4]. Surgical intervention is typically reserved for patients with uncontrolled pain. In these cases, formal spinal fixation and fusion carries a significant risk such as fixation and hardware failure, infection, wound complications, bleeding, and neurological injury due to marked bone weakness and the demographics of the patients themselves. This has called for minor interventions such as Vertebroplasty (VP) and Kyphoplasty (KP). These are minimally invasive interventions that are conducted as a day case surgery under sedation and strong analgesia. They have proven good outcomes specially regarding pain control in several studies [4,5].
On the other hand, vertebroplasty and kyphoplasty are not without complications. Many studies report about complications such as refracture, collapse and cement extravasation [2,4]. This has in turn called the need for adding segmental spinal fixation to them, while keeping the intervention as minimally invasive as it possible. Adding percutaneous spinal fixation to VP and KP has started to gain popularity among many surgeons, reporting an overall better clinical and radiological outcomes [6-10]. While there are only three studies comparing VP to VP plus percutaneous instrumentation [8-10] with a maximum of 2 year follow up, the aim of this study is to report our single center experience regarding the mid-term clinical outcomes, by comparing both techniques in 51 cases in order to add to the available little evidence regarding the efficacy and outcomes of each technique.
Materials and methods
Patients’ selection
This is a retrospective study analyzing the clinical and radiographic outcomes of cases who underwent vertebroplasty alone versus patients who received vertebroplasty plus percutaneous posterior spinal instrumentation for osteoporotic insufficiency fractures. After IRB approval, all the cases who were admitted for surgery for vertebral insufficiency fractures between January 2016, and January 2022 were identified and extracted from our databases, and examined against our inclusion and exclusion criteria.
Inclusion criteria
-Cases with vertebral insufficiency fractures, diagnosed with X-ray, CT or MRI and
-Cases with established osteoporosis (T Score less than -2.5), and
-Cases who received either vertebroplasty or vertebroplasty plus percutaneous instrumentation
Exclusion criteria
-Cases who had preoperative neurologic defecit
-Cases who have not completed a minimum of 1 year follow up
-Cases with a history of high energy trauma
A total of 69 cases with vertebral insufficiency fractures were extracted from our databases. Eighteen cases were excluded due to not fulfilling our selection criteria, leaving 51 cases for analysis and inclusion in this study. Patients were divided into two groups - VP group with 28 patients and VPPF group with 23 patients. Their demographic information is presented in table 1.
Table 1:
| VP group (28) | VPPF Group (23) | |
|---|---|---|
| Age (Mean + Range) |
68.2(53-79) | 71.6(49-84) |
| Sex | Females 22, Males 6 | Females 14, Males 9 |
| Comorbidities |
DM 5 cases Hypothyroidism 4 cases Chronic renal disease 1 case |
DM 5 cases Hypothyroidism 7 cases Hyperparathyroidism 3 cases |
| Body Mass Index (Mean+ Range) |
27.1 (18-36) | 29 (24-38) |
Surgical intervention
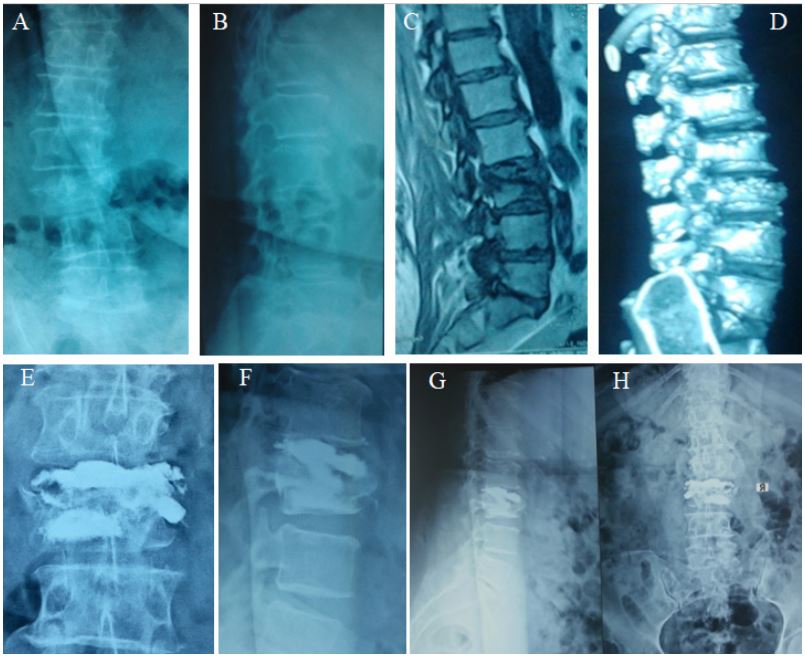
The same surgical team performed all the surgical procedures, and decision to perform VP or VPPF was at the discretion of the attending physician. In the VP group, surgery was performed under sedation and local anesthesia in a prone position utilizing orthogonal imaging with a C-arm. The vertebroplasty needle is inserted into the posterior one third of the fractured vertebra through the pedicles and a working channel is made. PMMA cement is injected slowly under fluroscopic guidance into the fractured vertebral body.
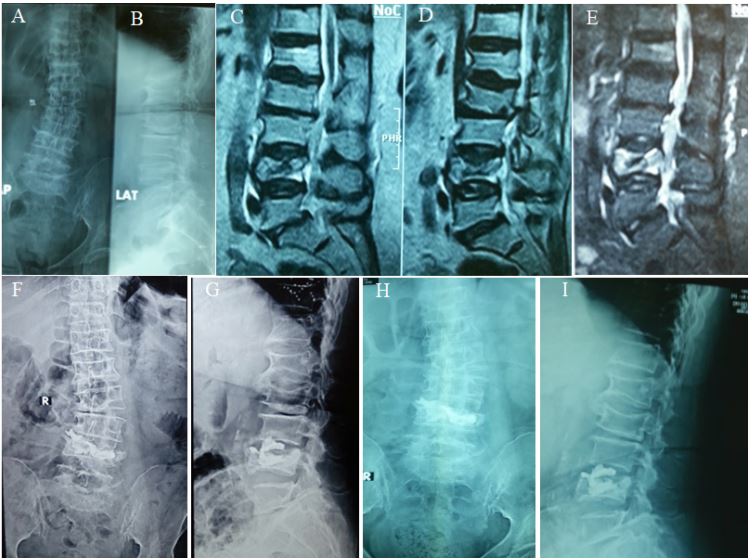
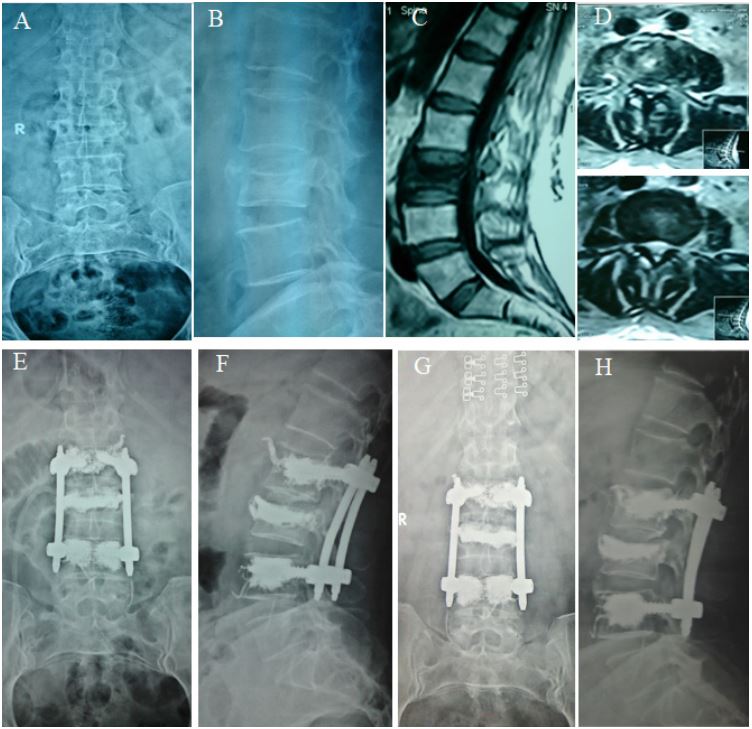
In VPPF group, it is performed under general anesthesia in prone position. Vertebroplasty was performed first in the same pervious way, then percutaneous posterior spinal instrumentation with pedicle screws was performed.
Post operatively, a dorso-lumbar brace was utilized consistent with the fractured level. Patients were followed up at 2,6 and 12 weeks, 3 months and then every 6 months up to 2 years. At every follow up X-rays were obtained.
Calcium, vitamin D and anti-osteoporosis medications were prescribed postoperatively for all patients in both groups.
Assessment of outcomes
Clinical outcomes were assessed using the Visual analogue scale [11] and the Oswestry Disability Index (ODI) [12] at each visit. The immediate postoperative radiographs in both groups were assessed for cement leakage, implants position, spinal alignment and reduction of the fractured vertebra. Any documented complication, such as infection, neurological compromise, refracture was extracted and recorded.
Statistical analysis
All statistical data were analyzed with MS Excel version 2208. Quantitative data are presented as the means and range. Statistical significance was defined as a p-value<0.05.
Results
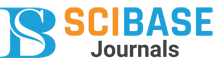
For the VP group, the mean follow up was 34.9±20.9 months, while for the VPPF group, the mean follow up was 39 ±15.5months, (P>0.05). The mean follow up in all the study cohort is 36.7±18.6 months. Significant differences were found in the operation time, blood loss and total length of stay between the two groups, with better values in the VP group (Table 2). No significant differences were found between the two groups in the preoperative and last follow up VAS, while there was a slightly better ODI in the VPPF at the final follow up. Mechanical complications such as refracture, progression of kyphosis and re-collapse occurred only in the VP group, while wound complications occurred only in the VPPF group. Cement leakage occurred more in the VP group (Table 2).
Table 2:
| VP(N=28) | VPPF(N-23) | P value | |
|---|---|---|---|
| Surgery duration (Min) | 41.7±9.3 | 96.3±21 | ˂0.0001 |
| Blood loss (ml) | 7.6±4.19 | 77.8±42.8 | ˂0.0001 |
| Length of hospital stay | 1.8±0.9 | 3.7±1.1 | ˂0.0001 |
| VAS Preop VAS Last follow up |
7.7±1.8 2.4±2 |
7.3±1.4 2.3±1.5 |
0.3882 0.8437 |
| ODI preoperative ODI Last follow up |
71.4±9.7 15±6.9 |
76±9.8 10±7 |
0.0998 0.0137 |
|
Complications Wound infection Cement leakage New fracture Re-collapse (kyphosis progression) |
- 8 3 4 |
1 3 1 - |
Complications
One case of superficial wound infection that was managed using antibiotics and single superficial debridement was recorded in the VPPF group. Cement leakage into the disc space was observed in 8 patients in VP group and 3 patients in VPPF group. New fractures occurred in 3 patients in VP group and in 1 patient in VPPF group, requiring surgery. Re-collapse, with kyphosis progression occurred in 3 cases in the VP group and have not occurred in the VPPF group (Table 2).
Discussion
This is a retrospective study of 51 cases comparing vertebroplasty alone versus vertebroplasty plus percutaneous posterior spinal instrumentation for osteoporotic insufficiency vertebral fractures. After a mean follow up of 36.7 months, there was no significant differences in the VAS score, however there were slightly better ODI for the VPPF group. Higher incidence of mechanical complications was observed with the VP group, including new fractures, re-collapse with kyphosis progression and cement leakage. Meanwhile, VPPF group showed more blood loss, longer hospital stays, significantly longer surgery duration and increased incidence of wound infection.
Vertebral insufficiency fractures secondary to osteoporosis are common, with one occurring every 22 seconds worldwide in people over age 50 [13]. When left untreated, many patients may suffer significant disability secondary to deformities, which may lead to thromboembolic complications [13]. For management of such fractures, percutaneous Vertebroplasty and Kyphoplasty are the most used surgery, with significantly good outcomes in controlling pain and disability [4,14-16]. However, with increased number of cases receiving vertebroplasty and kyphoplasty, and with longer follow up available, many complications showed up as a specific complication to this category of surgery, including cement leakage, re-collapse of the operated vertebra, with an incidence reaching 38.9% [17], and refracture of the operated vertebra or the adjacent ones which has a reported incidence of 5% [18].
Since the introduction of combined percutaneous spinal fixation in addition to percutaneous bone cement injection by Pingel et al [19], few studies reported satisfactory results of this technique. Elmasry et al compared percutaneous kyphoplasty with and without percutaneous fixation and found that the fixation group had less chance for mechanical complication, despite having less range of motion [20]. Zhong et al [21] also found that the fixation group had less cement leakage, less collapse and overall, less revision, along with better functional scores. Wu et al [22] compared the two techniques and found the fixation group had significantly better VAS with less chance of re-collapse than the kyphoplasty only group. Two previous studies [8,9] retrospectively compared the two techniques and also found the fixation group to have longer correction, with less chance for re-collapse along with better clinical scores. In the current study, we have compared vertebroplasty to vertebroplasty with percutaneous fixation. Adding fixation improved the ODI score and led to less chance of mechanical complications such as refracture and re-collapse, despite having more incidence of wound complications.
As for radiological outcomes, in the VP group we had higher incidence of re-collapse and refracture in the VP group. The reason behind recurrent collapse of vertebrae after cement injection techniques has been attributed to the progression of osteoporosis [23], cement leakage into the disk [24] and the occurrence of vertebral cleft [25]. The area of vertebral cleft consists of necrotic bone and fracture callus, along with areas of avascular necrosis which do not withstand loads without additional screw fixation. This should call for the use of additional instrumentation, especially with the high degrees of osteoporosis [26].
This study has several limitations: being retrospective, nonrandomized and on a relatively small number of cases in each group. Also, the mean short term follow up in this study is a major limitation, as a longer follow up is required to assess the possible mechanical complications in both groups. However, being a single center study performed by the same surgeons makes the procedure more consistent.
Conclusion
Adding percutaneous fixation to vertebroplasty significantly decreased the incidence of mechanical complications and improved the overall outcome scores. However, this came at an expense of increased operative time, wound complication and need for secondary procedures. Treatment should be individualized based on patient characteristics.
Declarations
Conflicts of interest: None to declare.
Funding: None to declare.
References
- Muratore M, Ferrera A, Masse A and Bistolfi A. Osteoporotic vertebral fractures: predictive factors for conservative treatment failure. A systematic review. Eur Spine J. 2018; 27: 2565-2576.
- Heary RF, Kumar S. Decision-making in burst fractures of the thoracolumbar and lum¬bar spine. Indian J Orthop. 2007; 41: 268-276.
- Wood KB, Li W, Lebl DR, Ploumis A. Man¬agement of thoracolumbar spine fractures. Spine J. 2014; 14: 145-164.
- Sun H, Li C. Comparison of unilateral and bilateral percutaneous vertebroplasty for os¬teoporotic vertebralcompression fractures: a systematic review and meta-analysis. J Orthop Surg Res. 2016; 11: 156.
- McCall T, Cole C, Dailey A. Vertebroplasty and kyphoplasty: A comparative review of efficacy and adverse events. Curr Rev Musculoskelet Med. 2008; 1: 17-23.
- Huang D, Ying J, Xu D, Chen J, Liu J, Yu T, Zhuang Y, Zhou L. Comparison of Percutaneous Kyphoplasty with or without Pedicle Screw Fixation in Osteoporotic Thoracolumbar Vertebral Fractures: A Retrospective Study. Dis Markers. 2021; 2021: 4745853.
- Wei Q, Zhang X, Wu Y, Cui E, Liu Z. Efficacy of pedicle screw fixation and vertebroplasty treatment of severe osteoporotic thoracolumbar vertebral compression fractures in senior patients. Int J Clin Exp Med. 2020; 13: 9465-9472
- Li Z, Wang Y, Xu Y, Xu W, Zhu X, et al. Efficacy analysis of percutaneous pedicle screw fixation combined with percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures with kyphosis. J Orthop Surg Res. 2020; 15: 53.
- Gu YT, Zhu DH, Liu HF, Zhang F, McGuire R. Minimally invasive pedicle screw fixation combined with percutaneous vertebroplasty for preventing secondary fracture after vertebroplasty. J Orthop Surg Res. 2015; 10: 31.
- Wang N, Xu JZ, Chen EL, Zhao SJ, Quan RF. Effect observation of percutaneous pedicle screw fixation combined with percutaneous vertebroplasty for the treatment of osteoporotic thoracolumbar fractures Zhongguo Gu Shang. 2018; 31: 339-346.
- Chiarotto A, Maxwell LJ, Ostelo RW, Boers M, Tugwell P, et al. Measurement Properties of Visual Analogue Scale, Numeric Rating Scale, and Pain Severity Subscale of the Brief Pain Inventory in Patients With Low Back Pain: A Systematic Review. J Pain. 2019; 20: 245-263.
- Brodke DS, Goz V, Lawrence BD, Spiker WR, Neese A, et al. Oswestry Disability Index: A psychometric analysis with 1,610 patients. Spine J. 2017; 17: 321-327.
- Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006; 17: 1726-1733.
- McCarthy J, Davis A. Diagnosis and Management of Vertebral Compression Fractures. Am Fam Physician. 2016; 94: 44-50.
- Wang E, Yi H, Wang M, Huang C. Treatment of osteoporotic vertebral compression fractures with percutaneous kyphoplasty: a report of 196 cases. Eur J Orthop Surg Traumatol. 2013; 23: S71-S75.
- Wang F, Wang LF, Miao DC, Dong Z, Shen Y. Which one is more effective for the treatment of very severe osteoporotic vertebral compression fractures: PVP or PKP?. J Pain Res. 2018; 11: 2625-2631.
- Wang C, Zhang X, Liu J, Shan Z, Li S, et al. Percutaneous kyphoplasty: Risk Factors for Recollapse of Cemented Vertebrae. World Neurosurg. 2019; 130: e307-e315.
- Wei P, Yao Q, Xu Y, Zhang H, Gu Y, et al. Percutaneous kyphoplasty assisted with/without mixed reality technology in treatment of OVCF with IVC: A prospective study. J Orthop Surg Res. 2019; 14: 255.
- Pingel A, Kandziora F, Hoffmann CH. Osteoporotic L1 burst fracture treated by short-segment percutaneous stabilization with cement-augmented screws and kyphoplasty (hybrid technique). Eur Spine J. 2014; 23: 2022-2023.
- Elmasry SS, Asfour SS, Travascio F. Finite Element Study to Evaluate the Biomechanical Performance of the Spine After Augmenting Percutaneous Pedicle Screw Fixation With Kyphoplasty in the Treatment of Burst Fractures. J Biomech Eng. 2018; 140: 10.1115/1.4039174.
- Zhong W, Liang X, Luo X, Quan Z. Vertebroplasty and vertebroplasty in combination with intermediate bilateral pedicle screw fixation for OF4 in osteoporotic vertebral compression fractures: a retrospective single-Centre cohort study. BMC Surg. 2019; 19: 178.
- Wu J, Xu YQ, Chen HF, Su YY, Zhu M, et al. Percutaneous kyphoplasty combined with the posterior screw-rod system in treatment of osteoporotic thoracolumbar fractures. Indian J Orthop. 2013; 47: 230-233.
- Borgen TT, Bjørnerem Å, Solberg LB, et al. High prevalence of vertebral fractures and low trabecular bone score in patients with fragility fractures: A cross-sectional sub-study of NoFRACT. Bone. 2019; 122: 14-21.
- Meyer C, van Gaalen K, Leschinger T, et al. Kyphoplasty of Osteoporotic Fractured Vertebrae: A Finite Element Analysis about Two Types of Cement. Biomed Res Int. 2019; 2019: 9232813.
- Chongyan W, Zhang X, Li S, et al. Mechanism of formation of intravertebral clefts in osteoporotic vertebral compression fractures: An in vitro biomechanical study. Spine J. 2018; 18: 2297-2301.
- Dupuy DE, Palmer WE, Rosenthal DI. Vertebral fluid collection associated with vertebral collapse. AJR Am J Roentgenol. 1996; 167: 1535-1538.