SciBase Journals
SciBase Clinical and Medical Case Reports
ISSN 2691-7785
- Article Type: Case Report
- Volume 1, Issue 2
- Received: Sep 11, 2023
- Accepted: Oct 25, 2023
- Published Online: Oct 31, 2023
Stenting for Severe C7 Stenosis of Internal Carotid Artery (ICA) and Related Literature Review
Xiao-Dong Wang1 ; Jian-Ping Zhang1,2; Jin-Gang Bao1,2; Xin-Wei Zhu1,2; Ri-Le Wu1,2*
1Inner Mongolia Neuroscience Society, Hohhot, China.
2Inner Mongolia Hospital Cerebrovascular Department, Hohhot, China.
*Corresponding Author: : Ri-Le Wu
Inner Mongolia Hospital Cerebrovascular Department, Hohhot, China.
Email: wurile@hotmail.com
Abstract
Intracranial Atherosclerosis (ICAS) is a common cerebrovascular lesion worldwide and an important cause of stroke [1]. Nonmodifiable risk factors include age, gender, and genetics, with age being a key factor and atherosclerosis usually progressive, with no clinical manifestations until middle age. Ischemic Heart Disease (IHD) has increased fivefold among people aged 40 to 60. Before menopause, women are less prone to atherosclerosis than men, and the incidence of atherosclerosis is increased in postmenopausal women [2,3]. The inheritance of various genetic polymorphisms and the accumulation of family risk factors (such as diabetes and hypertension) create multiple conditions for the formation of atherosclerosis [4]. On the other hand, modifiable risk factors, such as smoking, hyperlipidemia, diabetes, and high blood pressure, can be improved by adjusting daily life. Studies have analyzed that white people are prone to extracranial arterial occlusive disease, while Asian, black and Hispanic people have a higher risk of intracranial atherosclerotic disease [1]. Therefore, the prevention of atherosclerotic disease, has been very urgent, to increase publicity, from the source to solve the problem.
Keywords: Intracranial atherosclerosis; Ischemic heart disease.
Citation: Xiao-Dong W, Jian-Ping, Jin-Gang B, Xin-Wei Z, Ri-Le W. Stenting for Severe C7 Stenosis of Internal Carotid Artery (ICA) and Related Literature Review. SciBase Clin Med Case Rep. 2023; 1(2): 1009.
Introduction
Inner Mongolia Autonomous Region Hospital is located in Hohhot, China. The cerebrovascular department is the key department of the hospital, which undertakes the heavy task of the prevention and treatment of cerebrovascular diseases in the western cities of the Inner Mongolia Autonomous Region, and also undertakes the scientific research tasks of the Inner Mongolia Neuroscience Society. Atherosclerotic diseases, especially vascular diseases of the nervous system, have a high incidence in the northern region. This is just one of the cases we’ve treated. Share and promote communication.
Case presentation
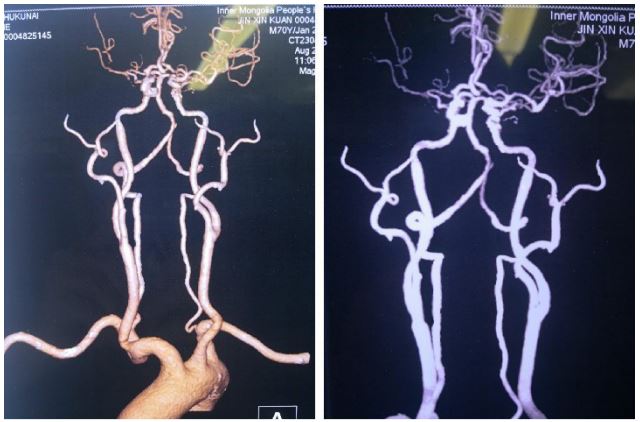
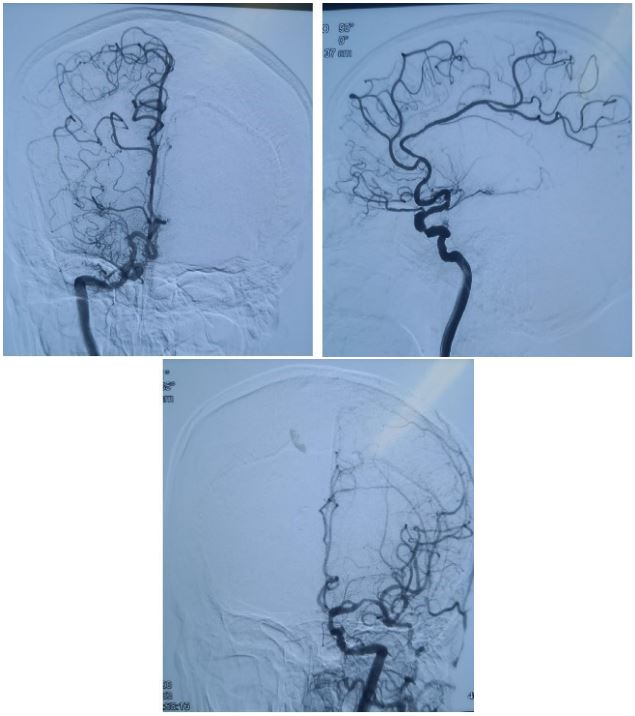
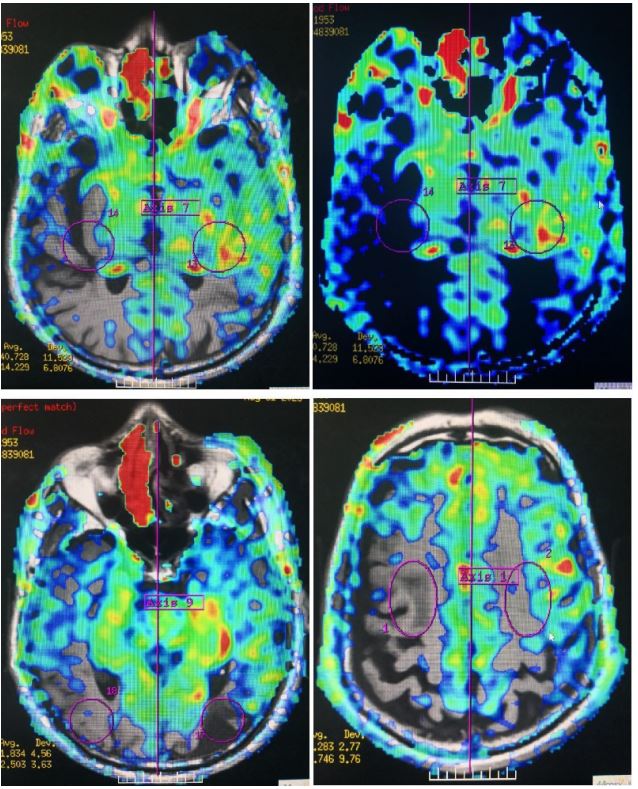
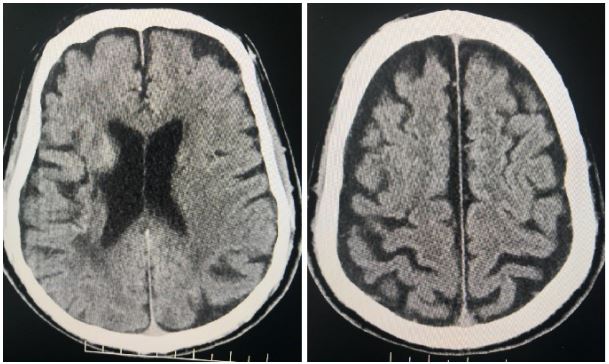
A 70-year-old male patient experienced sudden left limb weakness with progressive aggravation and dizziness 10 days ago. He was admitted to our hospital on August 29, and CTA indicated (Figure 1). 1) Aortic arch atherosclerosis 2) Non-calcified plaque in the distal segment of the Left Common Carotid Artery (LCCA) with mild luminal stenosis 3) Mixed and noncalcified plaque in the segment at the beginning of the Internal Carotid Artery (ICA) with bilateral common carotid artery bifurcation and mild luminal stenosis 4) Multiple calcification and mixed plaque in C2-6 segments of bilateral internal carotid arteries with mild to moderate stenosis 5) Small localized protrusions at segments C4 and 6 of the left internal carotid artery, excluding aneurysms; The M1 segment of the right middle cerebral artery was not developed, and occlusion was considered. 9) Limited lumen stenosis of the right anterior cerebral artery. Hypertension for more than 10 years. No diabetes, coronary heart disease. Neurological examination found muscle strength level IV in the left limb. Aspirin, clopidogrel bisulfate tablets, atorvastatin calcium tablets were given for antiplatelet and lipid-regulating plaque stabilization. On August 30, the patient was told to control diet and rest well after 10 PM. The nurse prepared the skin in the groin area and changed the operating clothes. The doctor ordered heparin sodium injection, uradil injection, lidocaine, dexamethasone and diphenhydramine. Cerebral arteriography was performed on August 31. The surgical procedures were as follows: supine position, routine disinfection and laydown of the right groin area, right femoral artery puncture after local anesthesia, insertion of 5F arterial sheath, 5F single bend angiography catheter guided by 0.035 wire, and left and right carotid artery and left and right vertebral artery angiography were performed respectively. The results suggested (Figure 2) that the right middle cerebral artery was occluded, the right internal carotid artery C7 segment was severely narrowed, the right vertebral artery compensated to the right brain through posterior circulation, the left carotid artery and the left vertebral artery were well developed, and no abnormalities were found in the venous system. After the operation, the artery sheath was removed and pressed for 15 minutes to stop bleeding and pressure bandaging. After operation, fluid rehydration prevented the occurrence of contrast nephropathy, uradil micropump was pumped to control blood pressure, the patient’s condition was stable, and surgery was scheduled. Prep for surgery on the morning of September 6. On September 7, percutaneous carotid stent implantation under general anesthesia was performed. The procedure was recorded as follows: Stenting with severe stenosis C7 segment of the right Internal Carotid Artery (ICA) was performed under general anesthesia. Lay the surgical sheet after disinfection. The 6F arterial sheath was inserted into the right femoral artery by puncture, and the 6F guided catheter was inserted into the C3 segment of the right Internal Carotid Artery (ICA) by a multifunctional catheter guide ribbon, and the Y-valve and three-way catheter were connected. The right Internal Carotid Artery (ICA) angiography was performed by continuous pressure infusion of heparin saline. 3,000 units of heparin intravenously. The guide wire (SYNCHR-14 300 mm) was sent to the A2 segment of the right Anterior Cerebral Artery (ACA), and the balloon (Gateway 3.5 mm × 9 mm 8 atm) was expanded at the stenosis, and the balloon was withdrawn, and the stenosis was significantly improved by angiography. The microcatheter (Excelsior XT-27 150 cm × 6 cm) was sent along the guide wire(SYNCHR-14 300 mm) to the right anterior cerebral artery at a distance of A3, the microcatheter was withdrawn, and the stent system (Neuro form-EZ 4.5 mm × 20 mm) was placed along the microcatheter at the stenosis. Release the support when the location is correct. Reimaging showed sufficient stent expansion (Figure 4). Intracranial angiography showed significant improvement in intracranial blood supply. The artery sheath was pulled out and the femoral artery was closed by the closure device. The patient was awake and answering questions correctly after surgery, but there was poor movement of the left limb. Intracranial thrombosis was considered. In order to confirm the diagnosis again, cerebral arteriography was performed, left femoral artery puncture failed, right femoral artery puncture was performed again, right carotid arteriography was performed after success, and microthrombus formation was found in the bifurcation of the right pericallosal artery, and distal blood flow was patency. Tirofiban 5 ml was immediately injected into the artery and observed for 10 minutes. The patient had correct answer. The muscle strength of the left upper limb was grade 4, and the muscle strength of the left lower limb was grade 3. After the patient returned to the ward from the operating room, brain CT examination showed no obvious abnormality (Figure 5), and Tirofiban was injected with 6 ml/h of micropump as the initial speed and gradually adjusted. On the morning of September 8, the muscle strength of the patient’s left limb returned to the level of muscle strength before admission and was gradually improving.
Discussion
The well-known SAMPPRIS study, the only randomized controlled trial to evaluate stenting plus optimal medication versus optimal medication alone in patients with symptomatic severe intracranial vascular stenosis, was terminated early due to high stroke rates in the interventional group. Since then, intracranial stenting has been considered as an alternative treatment option when the best drug therapy fails [5]. The recurrence rate of stroke within 1 year in patients with severe intracranial artery stenosis is as high as 12.2%, even with optimal drug treatment. At present, with the continuous progress of endovascular therapy technology and the scientific and efficient perioperative management, the success rate of intracranial stent therapy technology is getting higher and higher.
For patients with first or recurrent symptomatic intracranial large artery stenosis who failed medical treatment, the patient's medical history and related imaging examinations indicated severe C7 stenosis (≥70%) of the right anterior cerebral artery, occlusion of the right middle cerebral artery, multiple high signals of DWI in the right basal ganglia, and hypoperfusion of the right frontotemporal parietal lobe (Figure 2), and the patient presented with left limb weakness. Considering the involvement of hypoperfusion and artery-artery embolization mechanism, the right Anterior Cerebral Artery (ACA) is the responsible vessel for this ischemic event, and the disease still develops after regular medication, indicating intravascular interventional therapy, and stenting is feasible to improve the hypoperfusion status of the narrow distal end.
In this case, after stent interventional surgery and anesthesia, the patient showed immobility of the left limb, which was significantly weakened compared with that before surgery. Later, after puncture and angiography, the patient's limb activity returned to the preoperative state after active antithrombotic treatment, which was considered to be related to plaque detachment caused by stenting and hypoperfusion caused by reduced blood pressure under general anesthesia.
Therefore, intracranial stent implantation must strictly grasp the adaptation signs, and constantly explore and summarize in practice.
Conclusion
The relatively high complication rate of intracranial stents has become a bottleneck restricting the development of intracranialstents. SAMMPRIS studied the incidence of stroke and mortality within 30 days after Wingspan stenting, 6.6% after Neurolink balloon dilated stenting and 6.5% after Apollo stenting. Therefore, effective prevention and control of related complications can bring hope for interventional treatment of intracranial vascular stenosis. In this case, stent thrombosis occurred in the patient and followed the blood flow to the distal anterior cerebral artery. Angiography showed the presence of blood flow in the distal cerebral artery. The patient was given arterial injection of Tirofiban and continuous intravenous infusion, and the muscle strength of the patient was completely restored. We considered that the reason was the low management of anesthetic blood pressure, the poor blood supply of the right middle cerebral artery and the anterior cerebral artery, and the hypoperfusion of the distal side, which eventually led to transient ischemia. Fortunately, the treatment was timely, and the patient did not suffer catastrophic consequences, which is something we should be happy about.
Declarations
Funding: This work was supported by Natural Science Foundation of Inner Mongolia Autonomous Region [Grants number: 2021MS08108]; Science and Technology Project of Inner Mongolia Autonomous Region [Grants number: 2021GG0114].
Declaration of competing interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Wong LK. Global burden of intracranial atherosclerosis. Int J Stroke. 2006; 1: 158-9.
- Manson JE, Hsia J, Johnson KC, Rossouw JE, Assaf AR, et al. Women’s Health Initiative Investigators. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med. 2003; 349: 523-34.
- Poornima IG, Mackey RH, Allison MA, Manson JE, Carr JJ, et al. WHI and WHI‐CAC Study Investigators. Coronary Artery Calcification (CAC) and Post-Trial Cardiovascular Events and Mortality within the Women’s Health Initiative (WHI) Estrogen-Alone Trial. J Am Heart Assoc. 2017; 6: e006887.
- Miller DT, Ridker PM, Libby P, Kwiatkowski DJ. Atherosclerosis: The path from genomics to therapeutics. J Am Coll Cardiol. 2007; 49: 1589-1599.
- Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, et al. SAMMPRIS Trial Investigators. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011; 365: 993-1003.