SciBase Journals
SciBase Clinical and Medical Case Reports
ISSN 2691-7785
- Article Type: Research Article
- Volume 1, Issue 2
- Received: Sep 04, 2023
- Accepted: Oct 27, 2023
- Published Online: Oct 31, 2023
Association between Medical Coping Modes and Family Function among Older Adults with Hypertension
*Corresponding Author: : Wenwen Yang
The First Clinical Medical College, Lanzhou University, Lanzhou, Gansu, China.
Email: 1456452710@qq.com
Abstract
Background: Coping, an essential intermediary variable of psychological stress, may affect the process of disease, and alongside family function, has also been linked to patient quality of life. However, these have not yet been investigated in older adults with hypertension.
Objective: To investigate the correlation between medical coping modes and family function, and the associated factors among older adults with hypertension in China.
Methods: This cross-sectional study included 341 patients (135 men, 206 women) with a mean age of 75.16. Participants were recruited from three hospitals in China, the Medical Coping Modes Questionnaire and the Family APGAR Index Scale were used to collect dada. Data were analyzed using Pearson correlation and multiple linear regression analysis in SPSS 26.0.
Results: Medical coping ability included three dimensions: Confrontation (19.42±3.83), avoidance (14.37±3.02), acceptance– resignation (9.19±2.09), and family function (7.47±1.47) were insufficient in older adults with hypertension; further, family function was positively correlated with the confrontation dimension (p<0.05), and negatively correlated with the acceptance– resignation dimension (p<0.05).
Conclusion: Improving family function among older adults with hypertension could enhance confrontation and reduce acceptance–resignation. Family-centered intervention measures may assist in promoting coping ability and healthy behaviors among older adults with hypertension.
Keywords: Older adults; Hypertension; Coping mode; Family function; Cross-sectional study; Correlation analysis; Influence factor; Health care.
Citation: Yang W. Association between Medical Coping Modes and Family Function among Older Adults with Hypertension. SciBase Clin Med Case Rep. 2023; 1(2): 1010.
Introduction
Hypertension was not only a health problem but also a global financial problem. It has become a significant global health burden affecting nearly 30% of the global population. People older than 65 years had an increased risk of hypertension [1]. Data from 182 countries reported by the World Health Organization and the United Nations Development Programme showed hypertension prevalence rates ranging from 13% to 41% [2]. Hypertension among South Korean adults was 30.5%, with a higher prevalence rate in the older population and in men [3]. In China, more than half of older adults suffered from hypertension, with a prevalence rate of nearly 90% in people older than 80 years. Hypertension was the primary risk factor for stroke, myocardial infarction, and even cardiovascular death [4,5]. Therefore, the older adults with hypertension deserved more attention.
Medical coping modes and family function in older adults with hypertension
Coping was an essential intermediary variable of psychological stress, which was the subjective and emotional response produced by various stimuli. Coping referred to an individual’s effort to solve stress conflicts and reduce the emotional burden caused by stress [6]. Medical coping ability could distinguish the different coping modes of patients with different diseases, and different coping strategies could affect the process of disease [7].
Folkman et al. [8] compiled the Medical Coping Modes Questionnaire (MCMQ) and explored the psychological and behavioral factors associated with the three major coping modes adopted by patients during treatment: Confrontation, avoidance, and acceptance-resignation. It was found that coping behavior involved delicate and diversified expressions, and grasping its overall impact required a comprehensive approach. The MCMQ showed that coping responses differed between patients with life-threatening diseases (such as cancer and myocardial infarction) and those with non-fatal diseases (such as arthritis and dermatitis). The three coping strategies were related to multiple demographic, disease, and psychological variables [10]. Jiang et al. [11] translated the MCMQ into Chinese to survey patients with chronic diseases. The results revealed that the Chinese version had the same clinical application value as the english version. However, some studies have found that it was not conducive for treating and controlling chronic diseases [12,13]. Avoidance positively correlated with quality of life indicators in older adults with stroke, and provided psychological protection to some extent [14]. Another study showed that cognitive treatment, relaxation treatment, and emotional support can enhance patients’ mental status and coping mode [15]. Confrontation with hospitalized stroke patients affected the acceptance of disability in those patients [16].
Family function was an essential aspect of patient care and was a subjective way to explore patients’ degree of satisfaction with their families [9,8]. Similk et al. devised a family function questionnaire called family APGAR, which consisted of adaptability, partnership, growth, affection, and resolve. The Family APGAR was used to assess family resources and report data in a family problem-oriented record, allowing physicians to view the APGAR in clinical practice. However, some studies have suggested that the family APGAR cannot fully detect family dysfunction [17]. Well-being, family function, gender, education level, and age were crucial factors affecting self-management behaviors among older adults with hypertension [18], and family function was closely correlated with patients’ quality of life [19]. In addition, family function could indirectly improve sleep status and quality of life, and enhance patients’ rehabilitation [20]. A decline in family function could lead to postoperative cognitive dysfunction in patients [21],so the importance of family for patients’ mental health should be highlighted [22]. Moreover, one study found that family functioning was positively correlated with self-care status [23].
Most importantly, medical coping modes and family function have been correlated with patients’ quality of life; however, no findings related to older adults with hypertension have been reported.
Purpose
This study aimed to investigate the medical coping ability and family function of older adults with hypertension in China, and provide a basis for creating family-centered transitional care.
Materials and methods
Aims
This study aimed to: (1) investigate the medical coping modes and family function of older adults with hypertension, (2) determine the relationship between medical coping modes and family function, and (3) identify the factors associated with medical coping modes and family function.
Participants
A cross-sectional study was conducted, and participants were recruited from January to June 2022 in China. The inclusion criteria were as follows: (1) patients who met the diagnostic criteria for hypertension in older adults [5]; (2) patients had clear consciousness, clear language expression, some reading ability, or could communicate with the investigators; and (3) patients were willing to participate in this study.
The exclusion criteria were as follows: (1) patients diagnosed with a mental illness or a language communication disorder; (2) those diagnosed with other serious diseases such as malignant tumors, heart failure, or renal failure; and (3) those who stayed in older care institutions or were older apartment patients.
Sample size
The questionnaire comprised 25 items. Based on a sample size calculation method of 5~10 times and considering that 20% of the returned questionnaires may be invalid, 300 participants were required.
Data collection
A random cluster sampling method was used. The investigators set each hospital as a unit and randomly selected three hospitals in a specific city in China. Before the survey, the investigators explained the purpose of the study to the patients, asked them to sign informed consent forms, and determined the appropriate time for the investigation.
The investigators were members of a research group that had received relative training. They explained each item to the patients, and the patients completed the questionnaires. If the patients could not fill in the questionnaires by themselves, a research group member would read the questionnaire in a neutral tone and collect the data through interviews. Questionnaires were distributed and collected immediately.
Instruments
Medical Coping Modes Questionnaire (MCMQ)
The MCMQ was used to assess the coping characteristics of patients experiencing specific life events such as diseases. The questionnaire included three dimensions-confrontation, avoidance, and acceptance-resignation-with 20 items in total. Using the Likert scoring method, the items were scored from 1 to 4. The total score for each dimension was calculated; the higher the dimension score, the more inclined the individual was to adopt a coping mode. Cronbach’s α for the three dimensions was 0.69, 0.60, and 0.76, respectively, and the retest reliabilities of the three dimensions were 0.64, 0.85, and 0.67, respectively [8,11].
Family APGAR Index (APGAR)
The APGAR questionnaire evaluated family adaptation, partnership, growth, affection, and resolution. A three-point scoring method was adopted with the answers “often like this,” “sometimes like this,” and “almost rarely” scored as 2 points, 1 point, and 0 point, respectively. The scores for the five questions were added to obtain a total score: 7-10 points indicated good family function, 4-6 indicated moderately impaired family function, and 0-3 points indicated seriously impaired family function. The retest reliability was 0.80-0.83 [24].
Demographic characteristics
A general situation questionnaire was developed through a literature review according to the purpose and content of the study, which included general sociological and disease-related data.
Ethics approval and consent to participate
This study was approved by the hospital ethics committee and registered with the clinical trials registry. All patients provided written informed consent before the study. The authors were accountable for all aspects of this study, and ensured that any questions regarding the accuracy or integrity of any part of the study were appropriately investigated and resolved.
Data analysis
After collection, the questionnaires were uniformly numbered and recorded using Epidata 3.0. Data were expressed as frequencies and percentages. Measurement data were expressed as M±SD and analyzed using t-test, ANOVA, Pearson correlation analysis, and multiple linear regression. Statistical significance was set at p<0.05. Statistical analyses were performed by SPSS 26.0.
Validity and reliability/Rigor
In this study, assessment scales with good reliability and validity were selected, and the questionnaires were checked before measurement to determine whether the questions were adequately worded, clearly expressed, consistent with a Chinese cultural background, and understood by all participants. All investigators were trained and assessed on the survey tools, and asked questions to ensure that the same information was communicated to the respondents, who were provided with an instruction manual. During the on-site investigation, a supervisor was assigned to monitor the progress of the investigation and conduct remedial work on site. Furthermore, the supervisor checked the data after entry to ensure accuracy.
Results
Characteristics of participants
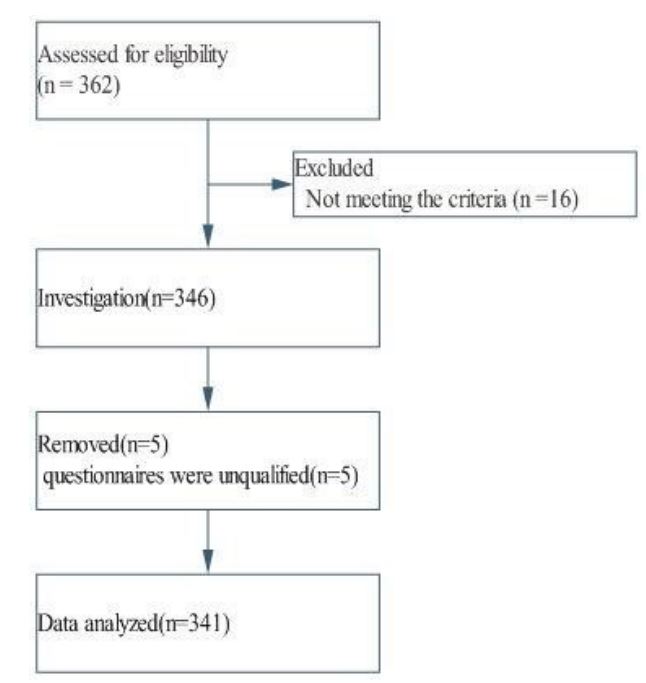
Between January and June 2022, 362 older adults with hypertension were recruited. Sixteen patients who did not meet the inclusion criteria were excluded. A total of 346 questionnaires were issued and collected, with an effective response rate of 100%. Five questionnaires were unqualified and removed; the final effective collection rate was 98.55% (Figure 1).
The average age of the 341 older hypertensive patients was (75.16±9.51) years (95% CI: 75.35-74.23). The sample comprised 135 men (39.59%) and 206 women (60.41%). Of the participants, 296 had healthy spouses (86.80%), 287(84.16%) were economically independent, and 311(91.20%) lived with family members (Table 1).
Medical coping modes and family function
In terms of medical coping modes, the score for the confrontation dimension was (19.42±3.83), for the avoidance dimension (14.37±3.02), and for the acceptance–resignation dimension (9.19±2.09). The overall score for family function was (7.47±1.47).
Analyses of medical coping modes and family function with different variables
The confrontation dimension differed significantly between older adults with hypertension according to sex, age, marital status, monthly income, primary caregiver, and payment method for health services (p<0.05). The avoidance dimension differed significantly between older adults with hypertension with different primary caregivers (p<0.05). The acceptance–resignation dimension differed significantly between older adults with hypertension according to sex, age, education, economic source, primary caregiver, and presence of concomitant chronic diseases (p<0.05). Family function differed significantly between older adults with hypertension according to sex, education, and monthly income (p<0.05; Tables 2 and 3).
Table 1: Characteristics of senile hypertensive patients in China (N=341).
| Variables | Frequency (%) |
|---|---|
| Age, mean (SD), years | 75.16(9.51) |
| Gender | |
| Male | 135(39.59) |
| Female | 206(60.41) |
| Education | |
| Primary school or lower | 90(26.39) |
| Junior middle school | 125(36.66) |
| Senior middle school/certificate | 111(32.55) |
| Bachelor’s degree/diploma or higher | 15(4.40) |
| Marital status | |
| Surviving spouse | 296(86.80) |
| Divorced or widowed | 45(13.20) |
| Monthly income (Yun) | |
| <2000 | 57(16.72) |
| 2000-2999 | 107(31.38) |
| ≥3000 | 177(51.91) |
| Economic sources | |
| Oneself | 287(84.16) |
| Direct relative | 42(12.32) |
| Collateral relatives | 3(0.88) |
| Social assistance | 9(2.64) |
| Primary caregivers | |
| Family members | 311(91.20) |
| Nanny | 15(4.40) |
| Living alone | 15(4.40) |
| Payment methods of health service | |
| Social health insurance | 297(87.10) |
| Self-financed | 35(10.26) |
| Free medical care | 9(2.64) |
| Types of concomitant chronic diseases | |
| 0 | 0 |
| 1 | 249(73.02) |
| 2 | 57(16.72) |
| ≥3 | 35(10.26) |
Table 2: Analyses of scores in medical coping mode and family function of senile hypertensive patients with different variables (mean[SD]).
| Variables | Confrontation | T/F value |
P | Avoidance | T/F value |
P | Acceptance resignation |
T/F value |
P | Family function |
T/F value |
P |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | 2.16 | 0.031 | 0.495 | 0.621 | 4.174 | 0 | 3.189 | 0.002 | ||||
| Male | 18.87±3.74 | 14.27±2.88 | 10.04±3.03 | 5.96±1.56 | ||||||||
| Female | 19.78±3.85 | 14.43±3.11 | 8.65±2.02 | 6.82±1.35 | ||||||||
| Age(years) | 4.109 | 0.007 | 2.504 | 0.059 | 10.343 | 0 | 1.462 | 0.225 | ||||
| 65- | 18.75±3.71 | 14.52±3.19 | 8.06±1.81 | 6.42±1.54 | ||||||||
| 75- | 20.34±4.05 | 14.78±2.85 | 9.88±2.29 | 6.88±1.38 | ||||||||
| ≥85 | 19.05±3.19 | 13.71±2.75 | 10.88±1.87 | 6.15±1.55 | ||||||||
| Education | 1.996 | 0.114 | 1.926 | 0.125 | 1.82 | 0.193 | 2.911 | 0.035 | ||||
| Primary school or lower | 18.91±3.63 | 13.87±2.43 | 9.83±2.34 | 6.70±1.49 | ||||||||
| Junior middle school | 19.67±3.88 | 14.83±3.08 | 9.13±2.05 | 6.02±1.44 | ||||||||
| Senior middle school/Cer- tificate |
19.54±4.03 | 14.29±3.38 | 8.64±1.96 | 6.65±1.49 | ||||||||
| Bachelor’s degree/diploma or higher |
21.20±3.09 | 14.01±2.45 | 9.01±2.27 | 7.60±1.80 | ||||||||
| Marital status | 3.671 | 0 | 0.489 | 0.625 | 1.079 | 0.281 | 0.661 | 0.303 | ||||
| Surviving spouse | 21.33±5.01 | 14.01±2.59 | 10.33±1.32 | 6.01±1.51 | ||||||||
| Divorced or widowed | 19.26±3.79 | 14.51±3.05 | 9.17±2.19 | 6.54±1.47 | ||||||||
| Monthly income (Yun) | 5.131 | 0.006 | 0.014 | 0.986 | 0.897 | 0.409 | 3.045 | 0.048 | ||||
| <2000 | 19.95±3.46 | 14.32±2.22 | 9.42±2.76 | 6.31±1.41 | ||||||||
| 2000-2999 | 18.45±3.99 | 14.35±3.12 | 9.44±2.44 | 6.06±1.53 | ||||||||
| ≥3000 | 19.83±3.78 | 14.39±3.18 | 8.98±1.99 | 6.78±1.42 | ||||||||
| Economic sources | 0.338 | 0.798 | 0.291 | 0.829 | 3.901 | 0.009 | 1.248 | 0.292 | ||||
| Oneself | 19.39±3.68 | 14.35±2.98 | 8.95±1.06 | 6.51±1.52 | ||||||||
| Direct relative | 19.64±3.72 | 14.36±2.44 | 10.51±3.08 | 6.29±1.27 | ||||||||
| Collateral relatives | 21.01±1.07 | 16.04±2.13 | 11.02±2.13 | 4.03±1.14 | ||||||||
| Social assistance | 18.67±2.05 | 14.33±3.14 | 10.33±3.28 | 7.09±1.73 | ||||||||
| Primary caregivers | 5.314 | 0.005 | 10.821 | 0 | 3.108 | 0.146 | 2.819 | 0.061 | ||||
| Family members | 19.59±3.73 | 14.55±2.98 | 9.15±3.08 | 6.57±1.39 | ||||||||
| Nanny | 16.40±5.84 | 11.01±3.14 | 11.01±3.53 | 5.81±1.03 | ||||||||
| Living alone | 18.80±1.52 | 13.80±1.21 | 8.41±1.59 | 5.21±1.04 | ||||||||
| Payment methods of health service |
9.439 | 0 | 1.106 | 0.332 | 1.405 | 0.247 | 0.405 | 0.668 | ||||
| Social health insurance | 18.50±2.99 | 13.99±2.81 | 8.85±1.14 | 6.49±1.43 | ||||||||
| Self-financed | 16.17±2.48 | 13.74±1.24 | 9.69±2.04 | 6.77±1.41 | ||||||||
| Free medical care | 18.77±2.72 | 15.12±0.83 | 8.78±1.27 | 6.00±1.87 | ||||||||
| Number of chronic diseases | 0.405 | 0.668 | 0.229 | 0.295 | 6.197 | 0.002 | 2.789 | 0.063 | ||||
| 1 | 18.29±2.93 | 14.02±2.59 | 8.62±1.79 | 6.69±1.29 | ||||||||
| 2 | 17.91±3.05 | 14.01±2.81 | 9.62±2.21 | 5.94±1.52 | ||||||||
| ≥3 | 18.65±4.09 | 13.71±2.99 | 9.89±2.21 | 6.08±1.11 |
Table 3: Correlation analysis of medical coping mode and family function of senile hypertensive patients (R).
| Variables | Family function | Confrontation | Avoidance |
|---|---|---|---|
| Confrontation | 0.188 a | ||
| Avoidance | 0.055 | 0.466 a | |
| Acceptance-resignation | -0.237 a | 0.107b | 0.252 a |
Note: a=P<0.01; b=P<0.05.
Table 4: Independent variable assignment table.
| Variables | Assignment |
|---|---|
| Gender | Male=1, Female=2 |
| Education |
Primary school or lower: 1; Junior middle
school: 2: Senior middle school/Certificate: 3; Bachelor’s degree/diploma or higher: 4 |
| Marital status | Surviving spouse: 1; divorced or widowed: 2 |
| Monthly income (Yuan) |
<2000: 1; 2000-2999: 2; ≥3000:3 |
| Economic sources |
Oneself: 1; direct relatives: 2; collateral
relatives: 3; social assistance: 4 |
| Primary caregivers | Family members: 1; nanny: 2; living alone: 3 |
| Payment methods of health service |
Social health insurance: 1; Self-financed:
2; Free medical care: 3 |
Table 5: Multiple linear regression analysis of medical coping mode and family function of senile hypertensive patients.
| Dependent variable |
Independent variable |
β | SE | β | T | P |
|---|---|---|---|---|---|---|
| Confrontation | (Constant) | 19.197 | 2.235 | - | 8.589 | 0.000 |
| Payment methods of health service |
-0.890 | 0.394 | -0.124 | -2.258 | 0.025 | |
| primary caregivers | -0.870 | 0.324 | -0.159 | -2.684 | 0.008 | |
| Avoidance | (Constant) | 17.431 | 1.940 | - | 8.986 | 0.000 |
| primary caregivers | -0.955 | 0.281 | -0.203 | -3.396 | 0.001 | |
| Acceptance- resignation |
(Constant) | 7.654 | 1.906 | - | 4.017 | 0.000 |
| Age | 0.052 | 0.016 | 0.177 | 3.160 | 0.002 | |
| Gender | -1.413 | 0.309 | -0.248 | -4.569 | 0.000 | |
| Primary caregivers | -0.955 | 0.281 | -0.203 | -3.396 | 0.001 | |
| Family function |
(Constant) | 6.060 | 1.773 | - | 3.418 | 0.001 |
| Gender | 0.754 | 0.288 | 0.151 | 2.619 | 0.009 | |
| Monthly income | 0.506 | 0.231 | 0.156 | 2.190 | 0.029 |
Discussion
Analyses of medical coping modes and family function scores
Coping was a vital intermediary variable for psychological stress. It represented an individual’s purposeful and conscious adjustment behavior in response to a changing environment [25]. In this survey, the scores of 341 older adults with hypertension for all dimensions of medical coping modes were lower than those of older patients with chronic disease in the community [25]. The scores in the confrontation and avoidance dimensions were higher than those of older patients with stroke [14], and the scores in the acceptance resignation dimension were lower than those of older patients with stroke [14] and chronic heart failure [23], which might be related to the inconsistency between the survey subjects and sites. The minimum history of hypertension for the participants was one year, the maximum history of hypertension was 30 years, and the average history of hypertension was (10.36±2.99) years. During the investigation, some patients expressed that they could communicate with medical staff, family members, relatives, and friends through various media platforms to understand disease-related knowledge and participate in treatment decisions. They indicated that they diverted themselves by watching TV and listening to music. However, during the interviews, some patients still thought that hypertension could not be cured; therefore, they needed to adhere to healthy lifestyle behaviors for the remainder of their lives. They also felt that they lacked the joy of life and confidence to control the disease and even adopted negative coping modes.
As an essential element in an individual’s life, family structure and function were closely related to health status and disease occurrence, development, and prognosis and operate as both causes and effects [25]. Good family functioning helped patients persist in treatment, relieve pressure, improve mood, and strengthen their confidence in conquering the disease. It also affected the health status and quality of life of family members. In this study, the score in family function was (7.47±1.47), indicating that the family function of older adults with hypertension was in the middle range. Among the patients, those with severe family dysfunction accounted for 10.56%, those with moderate family dysfunction 32.55%, and those with good family function 56.89%.
Furthermore, more than 50% of the patients received support and help from their families, which was consistent with the survey results of Hou et al. [20]. Of the 341 patients in this survey, 91.20% lived with family members, most of whom were their children or spouses. However, some spouses were older and weaker, had chronic diseases, and had insufficient nursing capacity. Patients and their families were concerned about taking medication, paying for treatment, and seeking medical advice. Family members must help patients improve their ability to cope with diseases, maintain a good mental state, and participate in recreational activities. Hypertension was a chronic physical and mental disease, and patients required regular, long-term drug treatment and good disease management.
Regarding the statistically significant differences found in the confrontation dimension, female patients and those over 75 years old, married, with a monthly income of more than 3,000 yuan, living with family members, or with government insurance could adopt a more positive coping mode such as confrontation. This might be related to the higher participation and compliance rates of women. Patients aged over 75 years had adapted to coexisting with hypertension. In addition, adequate payment methods for health services were conducive to reducing the financial burden caused by the disease and enabling patients to cope better.
Regarding the significant differences found in the avoidance dimension, the avoidance dimension scores of patients living with relatives and friends were higher; avoidance referred to avoiding stressful events. When patients were indifferent to the existence or severity of stressful events, this could help them shift their attention, divert negative emotions caused by the disease, and promote physical and mental health to some extent [26]. Older adults preferring to live with family members and enjoy family happiness might be related to traditional Chinese customs. Living with family members ensured that patients could effectively communicate with them to divert their attention and receive support. Care from a caregiver was a form of financially oriented care that lacked family affection and thus may have led to a low score.
Regarding the significant differences found in the acceptance-resignation dimension, it was found that older male patients and those with a bachelor’s degree or above, financial sources from collateral relatives, long-term care by a caregiver, or more than three concomitant diseases scored higher in the acceptance–resignation dimension. This might be related to the fact that male patients had a low compliance rate. Additionally, the self-care ability of older patients was insufficient, the patients with poor economic conditions relied on collateral relatives and thus lacked economic security, long-term care by caregivers could mean a lack of the emotional support generally provided by blood relations, and patients with more than three diseases might have felt inadequate in their ability to cope.
Female patients with a bachelor’s degree or higher or a monthly income of more than 3,000 yuan achieved a higher score in family function. This might be because older women in China have traditionally been in charge of family affairs, providing family care, and communicating effectively with family members. Patients with a higher educational level also had a better understanding of the disease, and might be able to better rationalize the relationship between the disease and the family. Additionally, economic security was more conducive to family function.
Confrontation was a positive coping mode conducive to establishing good self-management behaviors in older adults with hypertension. Acceptance-resignation, however, was a negative coping mode. Based on the low positive correlation between family function and the confrontation dimension and the low negative correlation between family function and the acceptance-resignation dimension revealed by the pearson correlation analysis, it was suggested that developing family function may improve the ability of older adults with hypertension to face disease and reduce the acceptance-resignation dimension, thereby improving their ability to cope with the disease. Multiple linear regression analysis indicated that, based on a traditional Chinese family, age, sex, primary caregivers, and payment methods for medical services should be considered when developing a family-community-hospital transitional care plan [27].
This study had some limitations. First, the participants were older adults with hypertension admitted in hospitals. Patients who could not communicate and those who had to stay in bed for long periods were excluded. Second, the study area was limited and no multicenter study was performed because of the limited workforce and funding. Finally, this cross-sectional study could not explain the causal relationship between medical coping modes and family functioning.
Conclusion
Older adults with hypertension have poor coping abilities and family function. Family functioning was positively correlated with the confrontation dimension and negatively correlated with the acceptance-resignation dimension. Age, sex, payment methods for health services, and primary caregivers affected family function and medical coping modes. Hence, it is necessary to consider various factors and develop interventions to improve disease-coping abilities and family functioning in older adults with hypertension.
References
- Yan S, Zheng QH, Sun DM, Wu Y, Li TM, et al. Diagnostic and Predictive Values of LAP in Hypertension: A Cross-Sectional Study in Chinese Population Older Than 65 Years. International Journal of Hypertension. 2021.
- Zeng Z, Chen J, Xiao C, Chen W. A Global View on Prevalence of Hypertension and Human Develop Index. Ann Glob Health. 2020; 86: 67.
- Kurjogi MM, Vanti GL, Kaulgud RS. Prevalence of hypertension and its associated risk factors in Dharwad population: A crosssectional study. Indian Heart J. 2021; 73: 751-753.
- Analysis of the aging process of Chinese population, the rising prevalence rate of chronic diseases among residents and the rising trend of per capita medical care consumptive expenditure of urban residents in 2018.
- Hypertension Branch of Chinese Geriatrics Society, N.C.R.C.f. G.d.C.A.o.G.C.D. Chinese guideline for the management of hypertension in the elderly. China Journal of Multiple Organ Diseases in the Elderly. 2019; 18: 81-105.
- Jiang GJ, Lu HS, Lou ZS, Yang AR, Cheng H, Mao ZX, et al. Psychological stress: Classification of coping and mental and physical health. China Mental Health Journal. 1993; 7: 145-147.
- ZJ, Z. Manual of Behavioral Medicine Scale. Beijing: Chinese Journal of Behavioral Medical Science. 2001; 253-254.
- Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. J Pers Soc Psychol. 1986; 50: 992-1003.
- Feifel H, SS, Nagy VT. Degree of life-threat and differential use of coping modes. Journal of psychosomatic research. 1987; 31: 91-99.
- Feifel H, Strack S, Nagy VT. Coping strategies and associated features of medically ill patients. Psychosom Med. 1987; 49: 616-625.
- Shen XH, JG. Report of 701 cases tested by Chinese version of the Medical Coping Modes Questionnaire. Chin J Behav Med and Brain Science. 2000; 9: 18-20.
- Ding F, YS. Correlation between disease coping mode and health function loss degree in elderly patients with chronic diseases. China Journal of Gerontology. 2017; 37: 3342-3343.
- Ren Y, JJ, Wen L, Xia HO. Study on correlation between self-efficacy and coping mode in elderly patients with chronic diseases. Chinese Journal of Modern Nursing. 2010; 16: 1301-1302.
- Mu YY, Zhou JX, Liu Y, Wang HJ, Hang GC, et al. Effects of social supports and coping modes on the qualities of life of elderly stroke patients. . China Journal of Gerontology. 2014; 25: 4047-4048.
- Shen X, Zhu X, Wu Y, Zhou Y, Yang L, et al. Effects of a psychological intervention programme on mental stress, coping style and immune function in percutaneous coronary intervention patients. PLoS One. 2018; 13: e0187745.
- Chai Q, YZ, Jin Y, Zhang Q. Factors influencing acceptance of disability among stroke patients in Tianjin, China:A cross-sectional study. euroscience Rehabilitation. 2016; 38: 37‐44.
- Gardner W, Kelleher KJ, Werner JJ, Farley T, Stewart L, et al. Does the family APGAR effectively measure family functioning? The Journal of family practice. 2001; 50: 19-25.
- Zhang XN, QC, Zheng YZ, Zang XY, Zhao Y. Self-management Among Elderly Patients With Hypertension and Its Association With Individual and Social Environmental Factors in China. The Journal of cardiovascular nursing. 2020; 35: 45-53.
- Qi HX, JC, Zhang ZJ, Feng XQ, Zhang JM. Correlation between family care degree and quality of life in coronary heart disease patients with cardiac insufficiency. General Practice. 2012; 15: 834-836.
- Hou RY, WL, Gao YX. Correlation between sleep quality and family care degree in elderly patients with essential hypertension. China Journal of Gerontology. 2015; 35: 2802-2803.
- Tao WP, MQ, Yang JP. The relationship between family care degree and postoperative cognitive dysfunction in patients undergoing spinal surgery. China Journal of Behavior Medecine and Brain Science. 2013; 22: 980-910.
- Yang L, Zhao QL, Liu HL, Zhu XM, Wang KX, et al. Family Functioning Mediates the Relationship Between Activities of Daily Living and Poststroke Depression. Nursing Research. 2021; 70: 51-57.
- Shi XQ, CW, Wu BW, Zhao HR, Huang Y. Correlation between family care and self-care in heart failure pafients. Chinese Journal of Modern Nursing. 2015; 21: 3126-3128.
- GS. The family APGAR: A proposal for a family function test and its use by physicians. The Journal of family practice. 1978; 6: 1231-1239.
- Ren Y, JJ, Wen L, Xia HO. Study on correlation between self-efficacy and coping mode in elderly patients with chronic diseases. Chinese Journal of Modern Nursing. 2010; 16: 1301-1302.
- Yui CX, WJ, Shen Z, Cai SL. Investigation on relationship between family function and quality of life for elderly stroke patients. Chinese Journal of Modern Nursing. 2008; 14: 2966-2968.
- Cooper J, Zimmerman W. The effect of a faith community nurse network and public health collaboration on hypertension prevention and control. Public Health Nurs. 2017; 34: 444-453