SciBase Journals
SciBase Clinical and Medical Case Reports
ISSN 2691-7785
- Article Type: Research Article
- Volume 1, Issue 3
- Received: Oct 27, 2023
- Accepted: Nov 29, 2023
- Published Online: Dec 06, 2023
Challenges and Practices in Modern Hand Surgery Nursing
Zhang Chan1; Chen Shouping2*
1Renhe Hospital, Changsha, Hunan, 410004, China.
2Ringbone Orthopedic Hospital, Changsha Hunan, 410004, China.
*Corresponding Author: Chen Shouping
Ringbone Orthopedic Hospital, Changsha Hunan, 410004, China.
Email: 1094426728@qq.com
Abstract
Purpose: This study aims to explore the changes in the patient spectrum and the challenges and practices in nursing brought about by the evolution of modern hand surgery patients and medical development.
Methods: A retrospective study was conducted on clinical data from 21,512 hand surgery patients in our hospital over the past 15 years. The study examined changes in patient spectrum, shifts in patient demands, evolutions in nursing models, and variations in patient satisfaction.
Results: The patient spectrum exhibited variations, accompanied by changes in patient demands and corresponding adjustments in nursing approaches. To address the challenges in hand surgery nursing, comprehensive training, rigorous assessments, skill enhancement, emphasis on practical effectiveness and proficiency, and continuous adaptation were employed as measures. These bold practices significantly improved the quality of nursing care.
Conclusion: Practice has shown that changes in the patient spectrum have posed challenges to nursing, which, in turn, spurred innovative thinking, refreshed perspectives, and promoted the development of nursing work.
Keywords: Nurse; Nursing; Hand surgery; Spectrum evolution; Challenges; Practice.
Citation: Chan Z, Shouping C. Challenges and Practices in Modern Hand Surgery Nursing. SciBase Clin Med Case Rep. 2023; 1(3): 1013.
Introduction
The development of modern hand surgery nursing is rooted in continuous innovation and progress in medicine and nursing. Hand surgery nursing plays a pivotal role in the modern healthcare system, profoundly impacting patient safety and functional recovery. With the rapid advancement of scientific technology, the rapid accumulation of medical knowledge, and the continuous improvement of clinical practices, hand surgery nursing has evolved from simple nursing tasks into a highly specialized, diverse, and exceptional field. Throughout its development, it has faced key challenges and difficulties in nursing techniques, teamwork, patient care, and more. This article conducts a retrospective study on changes in the spectrum of hand surgery patients in our hospital over the past 15 years, changes in patient needs, evolution of nursing models, and changes in patient satisfaction. The findings are presented as follows:
Materials and methods
Clinical data
A retrospective analysis was conducted on the clinical data of 21,512 patients who received inpatient treatment in our hospital’s hand surgery department from January 1, 2008, to December 31, 2022, spanning a 15-year period.
Inclusion criteria: (1) All injuries involving the wrist joint and beyond, including injuries to the upper limb’s soft tissues proximal to the wrist joint, such as nerve, tendon, vascular injuries, and extensive skin and soft tissue injuries, excluding bone and joint injuries and burns within this range; (2) Presentation to the hospital within 72 hours of injury; (3) Complete case data.
Exclusion criteria: (1) Chronic old hand injuries; (2) Hand diseases, deformities, etc.; (3) Incomplete case data.
Research methodology
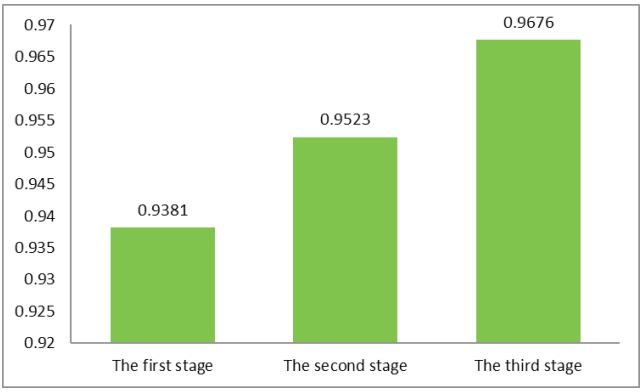
Considering the actual situation in our hospital and the completeness of data, this study defined three phases based on a 5-year interval. The first phase was designated as 2008- 2012, the second phase as 2013-2017, and the third phase as 2018-2022. Trained hand surgery physicians from our hospital organized and analyzed the medical records of eligible patients according to the inclusion criteria. This included collecting and analyzing data on patient demographics, injury characteristics, clinical nursing details, patient complaints, customer service management, and patient satisfaction surveys. From this data, we analyzed changes in the patient spectrum, nursing practices, and patient needs spectrum. We conducted a retrospective study on how the evolution of factors related to hand surgery over the course of 15 years impacted the stress, challenges, pain points, and difficulties in nursing work. We used these challenges as motivation to continually improve our capabilities, ensuring the sustained, healthy, and high-quality development of hand surgery nursing.
Statistical analysis
Statistical analysis was conducted using SPSS 20.0 statistical software. Categorical data were presented as percentages (%), and comparisons between samples were performed using the χ2 test. Continuous data were expressed as mean ± standard deviation (x±s), and comparisons between samples were carried out using the t-test. A significance level of P<0.05 was considered statistically significant.
Results
Basic characteristics
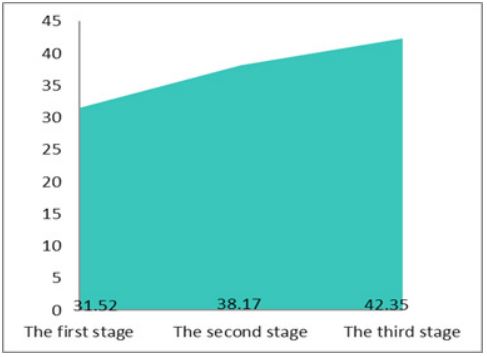
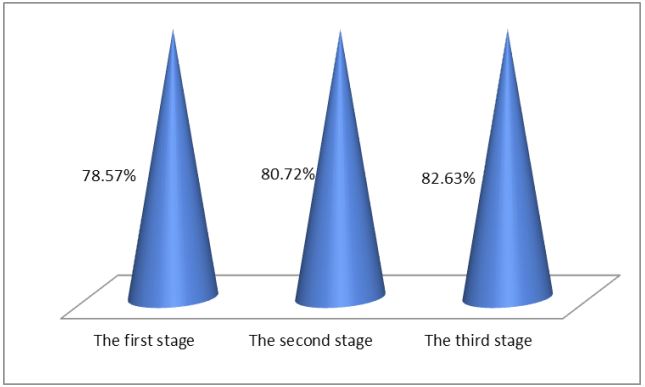
Over the period from 2008 to 2022, our hospital treated a total of 21,512 patients with hand injuries. Among them, there were 17,398 male patients (80.88%) and 4,114 female patients (19.12%), resulting in a male-to-female ratio of 4.23:1. The incidence of hand injuries was significantly higher in males compared to females (χ2 =6245.21, p=0.000). The age of the patients ranged from 5 days to 93 years, with an average age of (37.66±17.12) years. Specifically, the average age for male patients was (38.21±18.14) years, while for female patients, it was (35.49±21.65) years. There was a statistically significant difference in the distribution of gender across different age groups (χ2=21470.22, p=0.000).
Changes in patient spectrum
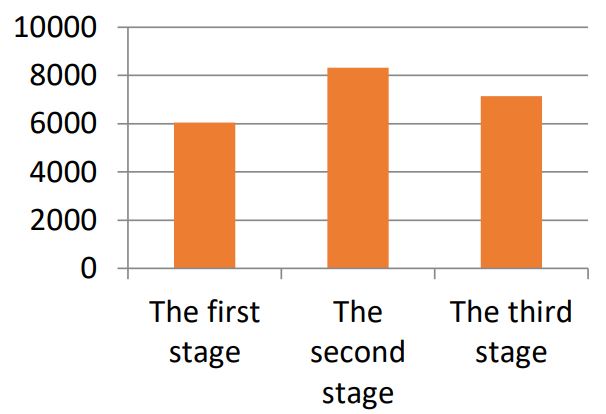
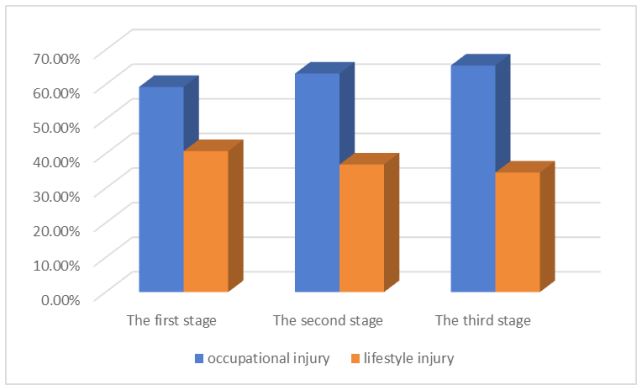
Statistical data indicate several notable trends in our hospital’s hand surgery patients over time:
Reduction in patient numbers: The number of patients treated in the hand surgery department gradually decreased, starting from the second phase. Increasing patient age: The average age of patients with hand injuries increased year by year. Rising proportion of male patients: The proportion of male patients showed a year-on-year increase. Occupational injuries highlighted: Occupational injuries gradually became more prominent compared to injuries resulting from daily life.
Evolution of patient needs spectrum
The spectrum of needs for orthopedic surgery patients continues to evolve along with advancements in medical technology, changes in nursing philosophies, and societal transformations. This evolution is characterized by: Safety needs: Surgical safety has become the primary concern for patients. They are concerned about the safety of the surgery itself, including sterile procedures, anesthesia safety, and the quality of surgical instruments. Pain management needs: Patients’ attention to pain has gradually increased. Post-operative pain often becomes a major concern for patients, making pain management a significant area of need. Personalized care needs: Contemporary orthopedic surgery patients place a growing emphasis on personalized care. They expect the healthcare team to thoroughly understand their medical history, pain experiences, and individual needs, in order to develop tailored care plans. Information and education needs: With the advent of the information age, orthopedic surgery patients have an increasing demand for information regarding the surgical process, post-operative care, and related aspects. They wish to receive detailed explanations and guidance to better understand and cope with the surgery. Rehabilitation and functional recovery needs: Modern orthopedic surgery patients are more focused on post-operative rehabilitation and functional recovery. They aim to regain their mobility as soon as possible, reduce post-operative complications, thus highlighting the importance of rehabilitation and recovery needs. Psychosocial support needs: The surgical process can have a significant impact on patients’ psychological and emotional well-being. As a result, psychosocial support has become an important requirement. Patients need emotional support, anxiety reduction, and psychological counseling.
Evolution of nursing spectrum
With the progress of society, advancements in medicine, and changes in the patient demographic, the nursing spectrum for orthopedic surgery patients has undergone rapid transformation. The scope of nursing care has evolved from general surgical nursing into a specialized and scientific development process, gradually moving towards a multidisciplinary and multi factorial integrated pattern of nursing development, encompassing fields such as society, medicine, and technology (Table 1).
Table 1: Evolution of nursing spectrum at various stages.
| Stage | Nursing content |
|---|---|
| First stage |
Basic nursing, wound care, post-operative
observation, pain management, mobility and
rehabilitation, fluid and nutrition,
psychological support, infection prevention, safety measures, education and guidance, and following medical orders. |
| Second stage |
The development of nursing technology, such as
remote monitoring, electronic health record
systems, virtual healthcare, personalized
care, interdisciplinary collaboration, psychological healthcare, comfort care, painless experiences, and functional rehabilitation, has been significant. Nurses are increasingly involved in clinical research, driving continuous innovation in nursing practice. |
| Third stage |
Preoperative preparation, operating room
nursing, Deep Vein Thrombosis (DVT) prevention,
postoperative monitoring, specialized wound care, drainage management, pain management and sedation, postoperative recovery, complications prevention and management, outcome assessment and documentation, and more. Modern technology applications, teamwork, close collaboration with physicians, anesthesiologists, physical therapists, and others provide comprehensive nursing support. |
Challenges arising from the transformation
Complex nursing demands
Modern orthopedic surgery patients have more complex nursing needs, involving various aspects such as the application of new equipment and instruments, pain management, rehabilitation promotion, psychological support, and more. The healthcare team needs to integrate multidisciplinary knowledge to provide more comprehensive nursing care.
Challenges in personalized care
Patients seek personalized care that caters to the diverse needs of individuals based on factors like gender, age, physical condition, and personal interests. This places higher demands on nurses’ communication, assessment, and planning abilities. Nurses need to understand the unique needs of each patient and create tailored care plans, ensuring that patients are in a state of physical, psychological, and emotional satisfaction and comfort.
Information and educational pressure
Patients’ demand for information about the surgical and nursing processes is increasing. They want to understand the treatment process for their condition, surgical procedures, potential complications, and treatment outcomes. The healthcare team must provide accurate, easily comprehensible information to encourage patient compliance with treatment while avoiding fear and anxiety. Therefore, nurses need comprehensive specialized knowledge and strong psychological counseling skills to address various patient inquiries and emotional changes.
Challenges in rehabilitation promotion
Rehabilitation promotion is a significant challenge in modern orthopedic nursing, requiring the facilitation of patients’ recovery in physical, psychological, social, and occupational aspects. The goal is to help patients regain their optimal condition, improve their quality of life, and, when possible, reintegrate into society and professional activities. Hence, the nursing team needs a comprehensive medical knowledge base and diverse skills. They must collaborate closely with physicians, anesthesiologists, physical therapists, and other interdisciplinary professionals to develop scientifically sound personalized rehabilitation plans for patients and diligently implement them to ensure the best rehabilitation outcomes.
Continuous improvement driven by transformation
The changes in factors such as the structure of orthopedic trauma patients, disease patterns, patient needs, and technological developments have prompted the renewal of orthopedic nursing concepts and innovative thinking. These changes have led to adaptations in nursing methods and strategies at our hospital to meet new demands, continually enhance the quality of care, and improve nursing outcomes. This, in turn, has further advanced the health and ongoing improvement of our hospital’s nursing practices.
Comprehensive training and rigorous assessment
As medical technology advances, orthopedic nursing goes beyond basic nursing skills, requiring nurses to possess broader knowledge and skills. Nurses need continuous professional training and learning to adapt to new nursing needs and technologies. Therefore, we have developed systematic training plans and strict assessment schemes. Training content: Training covers fundamental concepts of orthopedic nursing, aseptic techniques, basic knowledge of surgical instruments and equipment, practical skills such as aseptic procedures, surgical preparation, instrument handling, effective communication and interdisciplinary collaboration with multidisciplinary physicians, anesthesiologists, and other nursing staff, medical-patient communication techniques, operating room safety guidelines, accident response, infection control, and safety training. Practical skills are reinforced through simulated surgical environment exercises to enhance hands-on skills and emergency response abilities. Training methods: Various training methods are employed, including classroom training, simulation training, clinical practice, case studies, online training, role-playing, observation of actual surgeries, group discussions, case sharing, mentorship programs, and continuing education plans. Experienced senior medical and nursing staff, experts from higher-level hospitals and college professors serve as trainers. Additionally, training is conducted through activities such as “Party-Building Partnership” with higher-level hospitals, “Department Cooperation,” “Academic Exchange,” and “Academic Salon. Assessment and Evaluation: Evaluation methods include written tests, practical skills assessments, teamwork evaluations, and simulations of emergency situations. We establish “Technical Records for Continuing Education of Medical and Nursing Staff” and implement a “credit-based management” system, recording examination and assessment scores in these records, which are linked to individuals’ promotions and advancements.
Skill enhancement with a focus on effectiveness
Setting objectives: We establish personalized, phased work objectives based on the individual circumstances of nursing staff at different levels. These objectives clearly define the phased heights they aim to achieve in the field of orthopedic nursing, whether it’s improving specific skills or gaining deeper professional knowledge. Continuous learning: Recognizing that nursing is a constantly evolving field, we actively seek opportunities to participate in training, courses, seminars, etc., to continually acquire new knowledge and skills. Practical experience: Skills are honed through practical experience, including participation in simulated surgeries, observation of actual surgeries, or gradually accumulating experience in real surgeries. Reflection and feedback: After each practical experience, reflection is crucial. Analyzing one’s strengths and areas for improvement is essential. Seeking feedback from colleagues or mentors provides valuable suggestions and insights. Continuing education: Participation in continuing education programs ensures that nursing staff stay up-to-date with the latest developments, such as knowledge of the latest surgical techniques, instruments, and nursing guidelines. Problem-solving skills: When encountering challenges in their work, nursing staff actively engage in problem-solving, exploring different methods and solutions, and accumulating experience to enhance their abilities. Recognition and incentives: Through regular assessments and evaluations, exceptional performance is acknowledged and rewarded, while subpar performance may lead to criticism or penalties.
Mastering skills and keeping up with the times
Individualized care: Viewing each patient as a unique individual, considering their physiological, psychological, social, and cultural factors to create personalized care plans. This includes comprehensive patient assessment and, based on the assessment results, developing tailored medication management, treatment plans, rehabilitation programs, dietary advice, etc. Respecting patient choices, continuous monitoring, and adjusting care plans, while providing psychological support, education, and self-management. Focus on intra operative and postoperative care: Orthopedic surgery primarily involves brachial plexus anesthesia or local anesthesia, allowing nurses to communicate with patients while they are awake. This provides an opportunity to guide patients in adjusting their breathing rate, inquire about any discomfort during surgery, closely monitor vital signs, and take immediate action if any abnormalities are detected. Postoperatively, proper positioning is emphasized to facilitate venous return, avoid limb compression, and maintain limb warmth, promoting blood circulation and preventing swelling that could affect wound healing.
Pain management: Pain is the primary challenge patients face after orthopedic surgery. Pain can severely affect patients’ daily lives and rest, leading to sleepless nights, increased psychological burdens, negative emotions, and potentially prolonging hospital stays and increasing financial burdens. Therefore, pain management is a top priority. Nurses provide assistance to patients based on their actual conditions before, during, and after surgery, minimizing factors that may cause pain at each stage. For example, preoperatively, nurses explain the surgical process, share successful surgical examples, and encourage patients to build confidence, reducing anxiety and nervousness. Nurses aim to ensure that patients are in the best possible condition for treatment, avoiding psychological factors that increase pain perception. During surgery, gentle handling is emphasized. Postoperatively, wound infection checks are conducted regularly, communication with patients is maintained to keep their attention focused elsewhere, and patient-controlled analgesia pumps are introduced for effective pain relief. Patients are educated about the importance of pain management, and pain levels are assessed using Visual Analog Scales (VAS) and Numerical Rating Scales (NRS). Corresponding pain management measures are implemented based on the patient’s pain level. Nursing education: Diverse forms of education are provided to patients, such as verbal education by medical and nursing staff, informative pamphlets, educational videos broadcast on in-room televisions, science popularization articles and videos through mobile apps and We Chat public accounts, and QR codes for educational videos posted in patient rooms. These methods aim to enhance patients’ understanding of orthopedic diseases, treatment methods, and precautions, ensuring that patients fully comprehend and cooperate with treatment. Implementing a unified responsibility system: Nursing tasks are detailed based on the professional competence and years of experience of nursing staff. Entry-level nurses perform routine nursing tasks, such as changing dressings, bed linens, and measuring patients’ temperatures. Intermediate-level nurses are responsible for various therapeutic interventions, common complication prevention nursing, psychological counseling, and other tasks. These nurses have extensive nursing experience and can tailor interventions to individual patients, ensuring the effectiveness and specificity of nursing interventions. Nurse leaders monitor various nursing tasks, organize nursing summary meetings, analyze problems in daily nursing processes, and develop targeted solutions to enhance comprehensive nursing quality. Psychological intervention: Trauma often occurs suddenly, and most patients inevitably experience negative emotions such as tension and anxiety during the treatment process. These emotions can directly affect patients’ cooperation with nursing and treatment procedures. Nurses communicate with patients based on their specific conditions, educational levels, and professions, listening to their needs and providing patientcentered care. Patients’ questions are patiently answered, their psychological states are assessed correctly, trustful relationships are built, treatment compliance is improved, and negative emotions are alleviated, ultimately boosting patients’ confidence in their treatment. Enhanced interdisciplinary collaboration for early function recovery: Consultations with rehabilitation physicians are sought, and scientific rehabilitation exercises are adopted when the patient’s condition allows, facilitating early reintegration into normal social life.
These changes and efforts have significantly advanced orthopedic nursing at our hospital, better meeting patient needs, improving nursing quality, and rapidly advancing overall nursing and medical quality. Ward management, basic nursing, specialized nursing, critical patient care, nursing safety, and other indicators have met the standards. The quality of nursing documentation, health education, and patient satisfaction have also significantly improved. In the past five years, there have been no pressure ulcers, burns, falls from beds, falls, or other accidents. There have been no medical disputes or medical incidents.
Discussion
Hand injuries are a common type of injury worldwide. According to statistics from the U.S. Department of labor, hand injuries constitute the largest proportion of occupational injuries, accounting for 30% to 37% of all occupational injuries [1]. With social progress, technological advancements, and increased awareness among the public, the patient profile for traumatic conditions has undergone changes. Large-scale epidemiological data in this study indicate that over the past five years, the incidence of hand injuries has gradually declined, with the majority of patients being young and middle-aged males with work-related injuries, aligning with domestic reports [2,3]. The shifting patient profile poses challenges to nursing care. Nursing professionals must possess a solid foundation of basic and specialized knowledge, proficient technical skills, effective communication abilities, and a compassionate dedication to serving patients.
They need to continually update their knowledge, learn and master new technologies and information to meet the evolving needs of patients and clinical practice, thereby establishing a positive professional image for nursing personnel. Data suggests that the public holds a positive view of the roles of nurses and the nursing profession; however, there is still a lack of comprehensive understanding of nurses [4]. Therefore, nursing professionals and nursing managers should continuously enhance the image of nurses and increase public understanding and support for the nursing profession.
Currently, nursing approaches for hand surgery patients have expanded beyond routine care to include comfort care, rehabilitation training, psychological counseling, health education, clinical care pathways, and these methods have demonstrated positive nursing outcomes [5]. In response to new nursing challenges, we have focused on three major measures: comprehensive training with strict assessments, skill enhancement with a focus on practical effectiveness, and keeping pace with advancing skills to strengthen the foundation of knowledge and skills. When dealing with the psychological characteristics of young and middle-aged patients, we have also intensified psychological interventions. Nursing interventions seem to have a positive impact on preoperative anxiety in surgical patients [6].
The core of nursing work is to address the needs and concerns of patients. Nurses should respect patients’ personal values and cultural backgrounds, actively listen to their concerns and questions, and provide comprehensive, warm, and respectful nursing experiences. This includes establishing effective communication with patients, understanding their medical conditions and needs, assisting them in developing and implementing personalized nursing plans, and providing emotional and psychological support. Practice has shown that changes in patient demographics have brought challenges to nursing, stimulating innovative thinking, evolving nursing philosophies, and promoting the development of nursing care.
References
- Centers for Disease Control and Prevention (CDC). Nonfatal occupational injuries and illnesses among workers treated in hospital emergency departments- United States, 2003. Morb Mortal Wkly Rep. 2006; 55: 449-452.
- Chen SP. Clinical characteristics analysis of 5,302 hospitalized patients with hand injuries. Practical Medical Journal. 2016; 32: 1524-1527.
- Lin XJ, Chen SP. Retrospective study on clinical characteristics of hospitalized patients with hand injuries. Practical Journal of Hand Surgery. 2022; 36: 245-248.
- Wang W, et al. Survey on the current public awareness of the role of nurses and the nursing profession. Journal of Nursing. 2023; 38: 1-5.
- Liu P, Hu JJ, et al. Discussion on diverse nursing methods for postoperative care of hand surgery patients. Journal of Nursing Continuing Education. 2018; 33: 625-628.
- Ruiz Hernández C, Gómez-Urquiza JL, Pradas-Hernández L, Vargas Roman K, Suleiman-Martos N, et al. Effectiveness of nursing interventions for preoperative anxiety in adults: A systematic review with meta-analysis. J Adv Nurs. 2021; 77: 3274-3285.