SciBase Journals
SciBase Critical Care and Emergency Medicine
ISSN 2691-7785
- Article Type: Research Article
- Volume 1, Issue 1
- Received: Aug 17, 2023
- Accepted: Sep 29, 2023
- Published Online: Oct 06, 2023
Treatment Outcomes of Mechanically Ventilated Patients with COVID-19 and Associated Factors among Hospitalized Patients at ICU of SPHMMC, Addis Ababa, Ethiopia
Shimelis korbu1 ; Mariamawit Solomon2 ; Etsegent Aklog2 ; Ayalew Zewdie2 ; Derejit Mamo2 ; Yonas Keflegn2 ; Filagot Mesfin3 ; Alem Deksisa1*
1Adama Hospital Medical College, Adama, Ethiopia.
2Saint Paul Hospital Millennium Medical College, Addis Ababa, Ethiopia.
3Alert Hospital, Addis Ababa, Ethiopia.
*Corresponding Author: Alem Deksisa
Department of Public Health, Adama Hospital Medical College, Adama, Ethiopia.
Tel: +2519069074;
Email: alexdugna@gmail.com
Abstract
Introduction: Coronavirus (CoV) is derived from the word ‘corona’ meaning ‘crown’ in Latin. Coronavirus causes a range of human respiratory tract infections varying from mild cold to severe respiratory distress syndrome. Nowadays, due to the limited number of ICU beds and ventilators and the increasing number of patients with COVID-19 infection requiring MV data on patient characteristics, and outcomes of critical illness from COVID-19 are needed to inform decision-making about resource allocation, critical care capacity, and treatment of patients.
Objectives: To assess outcomes and associated factors of patients with COVID-19 on mechanical ventilation at SPHMMC COVID ICU, Addis Ababa, Ethiopia, 2020 G.C.
Methods: A single center cross-sectional study was used. All consecutive ICU admitted patients with RT-PCR confirmed COVID-19 and received mechanical ventilation support during the first 5 months were included. Data was collected from patient’s medical records using a structured questionnaire and the collected data was entered and analyzed using SPSS version 24.
Results: A total of 104 ICU patients with COVID-19 were included. The majority, 73.1% were male; the median age was 60 (IQR; 45-70) years, with 36.5% patients having at least one chronic medical condition. Out of 165, 104(63%) patients needed mechanical ventilation. Invasive and noninvasive ventilation were used in 93(89.4%) and 11(10.6%) patients, respectively. The most common treatments used by the patients were steroid (100%), antibiotics (99%) and vaso-pressors (57.7%). Experimental antiviral therapy was used in only 1% (n=1) of patients. Overall the ICU mortality was 14.6% and 88.5% among mechanically ventilated patients. Being fatigue (AOR=7.599; 95% CI: 1.65-35.12), IMV (AOR=5.28; 95% CI: 1.01-27.71), and septic shock (AOR=12.83; 95% CI: 1.46-13.11) were a significant risk factors for the ICU outcomes of the patients.
Conclusion: The study showed high proportion of mortality among ICU patients who received mechanical ventilator support with low rate of discharge. Male patients and old age groups with co-morbidity were disproportionately affected by the disease condition.
Keywords: COVID-19; SARS-CoV-2; Risk factors; Mortality; Mechanical ventilation.
Citation: Deksisa A, korbu S, Solomon M, Aklog E, Zewdie A, et al. Treatment Outcomes of Mechanically Ventilated Patients with COVID-19 and Associated Factors among Hospitalized Patients at ICU of SPHMMC, Addis Ababa, Ethiopia. SciBase Crit Care Emerg Med. 2023; 1(1): 1001.
Background
Corona contagion (CoV) is derived from the word ‘nimbus’; meaning ‘crown’ in Latin. It causes a range of mortal respiratory tract infections varying from mildly cold to severe respiratory torture patterns [1]. CoV are RNA contagions of the subfamily Corona virinae. They belong to the family Corona viridae and the order Nidovirales (nido Latin for ‘nest’). The subfamily Coronavirinae corresponds to nascence CoV, beta CoV, gamma CoV, and delta CoV grounded on the genomic structure. Corona contagions are a beta nimbus contagion that constitutes the subfamily Orthocoronavirinae, and family Coronaviridae [2].
Corona contagions (CoVs) are a group of largely enveloped contagions that are dissimilarly set up in humans and wildlife. With their high mutation rate and infectivity, CoVs are zoonotic pathogens that can infect creatures and humans, leading to 5- 10 acute respiratory runs. Piecemeal from infecting a variety of economically important invertebrates (similar to gormandizers and cravens), six species have been linked to beget complaint in humans [3-6].
The recent severe acute respiratory pattern (SARS-CoV-2) new nimbus contagion was linked in Wuhan, Hubei fiefdom of China in December 2019 by the Chinese center for disease and prevention which is taken from the throat tar of a case. Despite measures to contain the contagion, SARS-CoV-2 spread extensively across all mainlands in the ensuing months and the WHO declared the new nimbus contagion (COVID-19) outbreak as a global epidemic on March 11, 2020 [7,8]. As of December 2019 until May 7, 2020, the afflictions registered 3,886,2301,425 cases and 268,908 deaths in the world. Ethiopia has come among the COVID-19-affected countries as of March 15, the date on which one imported case was first detected. On May 7, 2020, there were 191 total notified cases and 4 deaths in Ethiopia [9]. Following the first SARS-CoV-2 outbreak in seafood and wildlife requests in Wuhan, secondary cases started to be linked after ten days. Although these new cases didn’t have any contact with the request, they had a history of contact with people who attended the request. Thus, also to SARS-CoV and doubtful to MERS-CoV, mortal-to-mortal transmission for SARS-CoV-2 has been reported and is presently considered as the main type of transmission worldwide that substantially occurs by inhalation of respiratory driblets spread by coughing or sneezing from an infected existent, but also by direct contact of defiled shells and also touching the nose, mouth, and eyes [10-12].
Clinical features varied from mild illness to severe or fatal one. The incubation period of the contagion varies from 2 to 14 days, and the main symptoms of the complaint include fever, cough, fatigue, foam product, briefness of breath, sore throat, and headache [3,13].
The Discovery of COVID-19 is grounded on the virological discovery by RT-PCR using hearties (nasopharynx, oropharynx), foam, feces, and also other suggestive attestations seen on casket radiographs and dynamic monitoring of seditious intercessors (e.g., cytokines). Utmost standard patterns observed on casket CT were ground-glass nebulosity, ill-defined perimeters, smooth or irregular interlobular septal thickening, air bronchogram, crazy-paving pattern, and thickening of the conterminous pleura [13,14].
Materials and methods
Study design and setting
Institution-based cross-sectional study design was conducted. This study was conducted at SPHMMC COVID ICU. St. Paul’s millennium medical college which is located at the capital city of Ethiopia was established through a decree of the Council of Ministers in 2010, although the medical school opened in 2007 and the hospital was established in 1968 by the late Emperor Haile Selassie. It is governed by a board under the Federal Ministry of Health. The college-initiated Ethiopia’s first integrated modular and hybrid problem-based curriculum for its undergraduate medical education and diversifying post graduate programs. The college has more than 2800 clinical, academic and administrative and supporting staffs that provide medical specialty service to patients who are referred from all over the country. The inpatient capacity is more than 700 beds and an average of 1200 emergency and outpatient clients are seen daily in the hospital prior to the pandemic.
The hospital was designated officially starting from June 8, 2020 G.C. as the national center for the management of COVID-19-infected patients in Ethiopia mainly serving the city and surrounding areas populations. It was re-purposed to have different compartments on already existing building, including an Intensive Care Unit (ICU), Semi-ICU, HDU and also male and female wards for treatment of patients at different level of illnesses which is assigned according to WHO criteria. The adult ICU has 13 beds with MV and dialysis machine. RT-PCR SARS-CoV-2– positive cases were admitted to the hospital. The initial decision to admit all patients to treatment center was because of the inconvenience of home isolation and management in many Ethiopian settings. Severe and critical cases were admitted to the ICU and Semi-ICU, whereas the others remained in the general ward and HDU. The care of COVID-19 patients is given by a multidisciplinary team composed of nurses, residents, laboratory technologists, pharmacists, internists, anesthesiologists, pulmonologist, emergency and critical care specialist and other supporting staff. The management of COVID-19 in the center is in line with the national and St. Paul’s treatment guideline.
The study was conducted on all consecutive ICU admitted patients with RT-PCR confirmed COVID-19 and received mechanical ventilation support from June 8 to October 11, 2020 G.C.
Sample size determination
Because of the small number of cases in ICU all consecutive ICU admitted patients with RT-PCR confirmed COVID-19 and received mechanical ventilation support from June 8 to October 11, 2020 G.C were included in the study.
Subjects
The sample was obtained by consecutively selecting all adult patients admitted to the ICU of SPHMMC with laboratory-confirmed COVID-19 infection by real-time reverse transcriptase PCR assay of naso/oropharyngeal swab specimens and received Mechanical ventilation during the study period. A total of 1127 patients were admitted with COIVD-19 infection to the hospital and of those 165 patients who required ICU level care (29%) were admitted to ICU and among these 104 patients who required mechanical ventilator support and fulfilled the eligibility criteria were included in the study.
Data collection
Data was collected from patient’s medical records using A Structured questionnaire in English language. The questionnaire was prepared by reviewing different literatures and undertaking modifications for the population studied. It was modified further after a pre-test and before the data collection. It was followed and reviewed during data collection. It was collected by trained data collectors in St. Paul’s hospital working at COVID treatment center and completeness was be checked by principal investigator. The information of all patients, including demographics, clinical presentation, laboratory parameters and patient outcomes was extracted from medical records. Laboratory parameters were divided into three categories: Hematologic and inflammatory biomarkers, coagulation factors and organ-injury biochemical biomarkers.
Data analysis
The collected data was cleaned, coded, and entered into EPI Data version 7.1 and then exported for analysis to SPSS version 24. The data were analyzed using binary and multivariate logistic regressions to determine the effect of various factors on the outcome variable. The results were presented in tables, figures, and text using frequencies and summary statistics such as standard deviation, mean, and percentage to describe the study population about relevant variables. The degree of association between dependent and independent variables was analyzed using an odds ratio with 95% confidence interval and p-value <0.05 declared statistical significance.
Results
Socio-demographic characteristics of respondents
A total of 1127 patients were admitted with COIVD-19 infection to the hospital and of those 165 patients who required ICU level care (29%) were admitted to ICU and among these, 104 patients who required mechanical ventilator support and fulfilled the eligibility criteria were included in the study. Of those, 12(11.5%) patients were discharged from ICU and 92(88.5%) patients were died in the ICU.
The median age of patients admitted in the ICU and received MV support was 60 years [IQR: 45-70], with 61 patients (58.7%) who were ≤64 years and majority 73.1% (76/104) of the patients were male (Table 1).
Table 1: Distribution of Socio-demographic characteristics of respondents who participated on risk factors and outcomes of patients with COVID-19 on mechanical ventilation at SPHMMC COVID ICU, Addis Ababa, Ethiopia from June 8 to October 11, 2020 G.C.
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Age group | 18-34 | 12 | 11.5 |
| 35-49 | 21 | 20.2 | |
| 50-64 | 28 | 26.9 | |
| 65-79 | 34 | 32.7 | |
| >=80 | 9 | 8.7 | |
| Sex | female | 28 | 26.9 |
| male | 76 | 73.1 |
Table 2: Clinical characteristics of patients on ICU admission of COVID-19 assessed on risk factors and outcomes of patients with COVID-19 on mechanical ventilation at SPHMMC COVID ICU, Addis Ababa, Ethiopia from June 8 to October 11, 2020 G.C.
| WHO criteria for disease severity | Mild | 11 | 10.6 |
|---|---|---|---|
| moderate | 10 | 9.6 | |
| severe | 27 | 26.0 | |
| critical | 56 | 53.8 | |
| Co-morbidity | none | 23 | 22.1 |
| 1 | 38 | 36.5 | |
| 2 | 27 | 26.0 | |
| >=3 | 16 | 15.4 | |
| Initial presenting symptoms | Dry cough | 67 | 67.70% |
| Productive cough | 18 | 18.20% | |
| Shortness of breath | 85 | 85.90% | |
| Chills/rigors | 11 | 11.10% | |
| Fever | 56 | 56.60% | |
| Fatigue | 71 | 71.70% | |
| Myalgia | 27 | 27.30% | |
| Malaise | 13 | 13.10% | |
| Arthralgia | 12 | 12.10% | |
| Chest pain | 12 | 12.10% | |
| Headache | 35 | 35.40% | |
| Vomiting | 17 | 17.20% | |
| Diarrhea | 2 | 2.00% | |
| Confusion | 26 | 26.30% | |
| Abdominal pain | 3 | 3.00% | |
| Sore throat | 3 | 3.00% |
Clinical characteristics
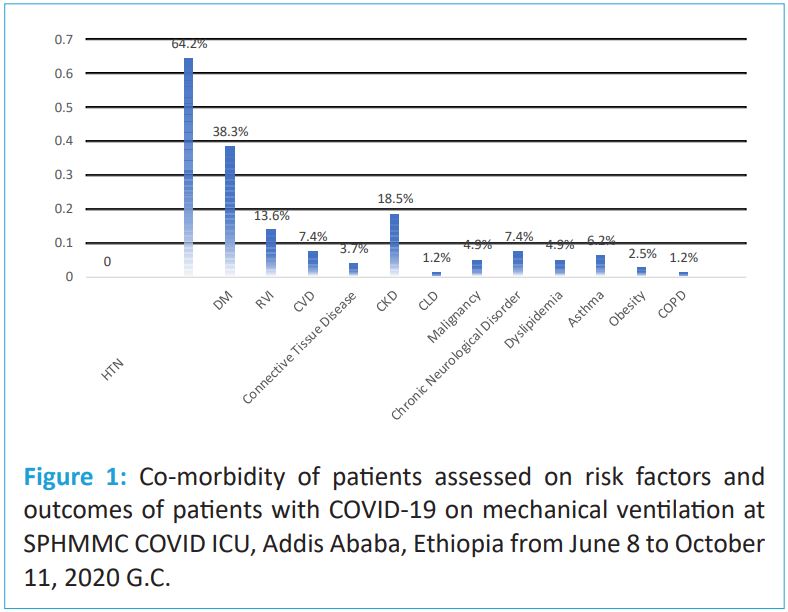
Among 104 patients admitted for MV support 38 (36.5%) patients had at least one co morbidity, the most common co morbidities were hypertension 52(64.2%) and diabetes 31 (38.3%) (Table 2 and Figure 1). According to WHO criteria for disease severity almost about half (53.8%) of patients were critical at the time of triage at treatment center as shown in table 2. Regarding presenting symptoms of patients to health facility the most common were SOB 85(85.9%), fatigue 71(71.7%), dry cough 67 (67.7%), fever 56(56.6%), and headache 35(35.4%) (Table 2).
Laboratory indices of patients on ICU admission
The most common laboratory abnormalities on ICU admission were leukocytosis (59 of 103[57.3%]), lymphocytopenia (82 of 103[79.6%]), neutrophilia (85 of 103[82.5%]), hyperglycemia (43 of 104[41.3%]) and low INR (37 of 71[52.1%]) of patients respectively.
More than half (65 of 103[63.1%]) of this cohort had normal platelet count. About one third (32 of 103[31.1%]) of patients had low hematocrit. Approximately one-quarter (23 of 101[22.8%]) and (22 of 101[21.8%]) of patients had hyponatremia and hyperkalemia respectively. Some patients demonstrated liver injury with elevated aspartate aminotransferase (AST; 36 of 99[36.4%]) and alanine aminotransferase (ALT; 25 of 99[25.3%]). Some of patients had kidney injury indicated by elevated plasma urea (39 of 102[38.2%]) and serum creatinine (39 of 102[38.2%]). Laboratory findings on ICU admission are summarized in Table 3.
Table 3: Laboratory findings on ICU admission of COVID-19 pa- tients assessed on risk factors and outcomes of patients with COVID-19 on mechanical ventilation at SPHMMC COVID ICU, Addis Ababa, Ethiopia from June 8 to October 11, 2020 G.C.
| Laboratory Indices | Total | Median |
|---|---|---|
| WBC (cells/ul) | 103 | 10.9 (7.3,14.4) |
| Lymphocytes cout (%) | 103 | 6.2 (4-10) |
| Neutrophil count (%) | 103 | 88.6 (81,91.6) |
| Platelet count (cells/ul) | 103 | 204 (145-264) |
| Hematocrit (%) | 103 | 40 (34.2-45.2) |
| AST (U/L) | 100 | 50.9 (32.93-78) |
| ALT (U/L) | 100 | 35.7 (24.93-58.95) |
| ALP (U/L) | 100 | 92 (70.25-121.75) |
| Urea (mg/dl) | 102 | 39.8 (26.68-104.53) |
| Creatinine (mg/dl) | 102 | 0.9 (0.75, 1.78) |
| Total bilirubin (mg/dl) | 65 | 0.34 (0.23, 0.67) |
| Glucose (mg/dl) | 103 | 182 (127, 234) |
| Na+ (mEq/L) | 101 | 137.8 (133, 140) |
| K+ (mEq/L) | 101 | 4.63 (3.83, 5.2) |
| PT, s | 78 | 16.05 (12.3, 18.63) |
| aPTT, s | 77 | 26.7 (22, 32.25) |
| INR 77 | 1.2 | (0.93, 1.61) |
Treatments and complications in hospital
Most patients 103 (99%) were treated with antibiotics and all the patients received systemic steroids in there stay in the treatment center. Vasopressor support was used for 57.7% of the patients, and the proportion of deceased patients who required vasopressor support was significantly higher than that in the discharged patients (64.1% vs. 8.3%, x2 =13.54, df=1, P<0.001). RRT was used in 17.3% of the patients, and out of these 3 of the patients who had preexisting CKD needed RRT. About 73(70.2%) of patients received therapeutic anticoagulation. Other experimental therapy was used by only one patient during the study period but no immunosuppressive therapy was used in the study population.
During the ICU stay among the study groups, 11(10.6%) patients received only non-invasive ventilation. 21(20.2%) patients were treated with non-invasive ventilation prior to endotracheal intubation. Thus, 93 patients (89.4%) over all received invasive mechanical ventilation, of whom only 12(11.5%) received neuromuscular blockade
During the study period about 97 patients developed at least one complication among these the most common were hospital acquired pneumonia (66[68%]), acute kidney injury (58 [59.8%]), septic shock (57[58.8%]), and suspected Pulmonary embolism (16[16.5%]) (Table 4).
Table 4: Treatments given and complications developed on ICU admission of COVID-19 patients on mechanical ventilation at SPHMMC COVID ICU, Addis Ababa, Ethiopia from June 8 to October 11, 2020 G.C.
| Variables | Categories | Frequency | Percentage |
|---|---|---|---|
| Treatment given | Vasopressors | 60 | 57.7% |
| RRT | 18 | 17.3% | |
| Therapeutic anticoagulation | 73 | 70.2% | |
| Antibiotic therapy | 103 | 99.0% | |
| Antifungal therapy | 8 | 7.7% | |
| Antiviral therapy | 1 | 1.0% | |
| Glucocorticoid therapy | 104 | 100.0% | |
| NMBA | 12 | 11.5% | |
| Experimental therapy | 1 | 1.0% | |
| Non-invasive ventilation | 11 | 10.6% | |
| Invasive mechanical ventilation | 93 | 89.4% | |
| Complications | Heart failure | 3 | 3.1% |
| Cardiac arrest | 3 | 3.1% | |
| Myocardial infarction | 4 | 4.1% | |
| Deep venous thrombosis | 2 | 2.1% | |
| Diffuse intravascular coagulopathy | 6 | 6.2% | |
| Septic shock | 57 | 58.8% | |
| Liver injury | 9 | 9.3% | |
| AKI | 58 | 59.8% | |
| Gastrointestinal hemorrhage | 9 | 9.3% | |
| PTE | 16 | 16.5% | |
| Pneumothorax | 5 | 5.2% | |
| HAP | 66 | 68.0% | |
| VAP | 3 | 3.1% | |
| Cardiac dysrhythmia | 10 | 10.3% | |
| CAUTI | 2 | 2.1% |
Treatment outcomes of mechanically ventilated clients
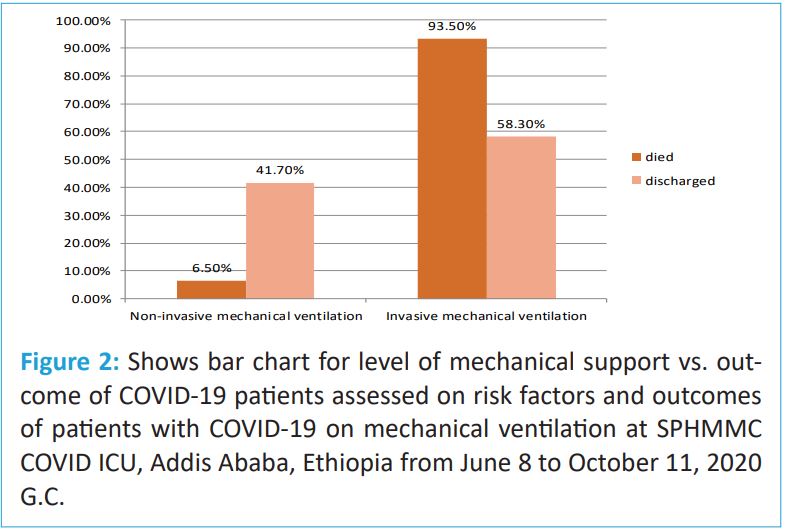
At the study’s cutoff date of the entire cohort, 165(14.6%) were admitted to the intensive care unit with the overall ICU mortality of 102(61.8%) and 104(63%) patients received mechanical ventilation. Among the 104 patients who received mechanical ventilation, 92(88.5%) died, 12(11.5%) were discharged from ICU (Figure 2).
Table 5: Risk factors for the outcomes of patients with COVID-19 on mechanical ventilation at SPHMMC COVID ICU, Addis Ababa, Ethiopia from June 8 to October 11, 2020 G.C.+
| Variableks | Treatment outcomes | Crude OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|---|---|
| Discharged alive | Died | |||
| Age | ||||
| 18-34 | 3 | 9 | 4.02 (0.83-19.38) | 0.40 (0.70-2.28) |
| 35-49 | 3 | 18 | 0.89 (0.22-3.56) | 0.52 (0.09-2.99) |
| 50-64 | 4 | 24 | 0.33 (0.04-2.69) | 1.04 (0.17-6.49) |
| 65-79 | 1 | 33 | 2.11 (0.70-5.59) | 0.38 (0.06-2.39) |
| >=80 | 1 | 8 | 1:00 | 1:00 |
| Fatigue | ||||
| Yes | 3 | 68 | 8.5 (2.12–4.03)** | 7.59 (1.65–5.12)** |
| No | 9 | 24 | 1:00 | 1:00 |
| Days from symptom onset to ICU admission | ||||
| <5 | 6 | 25 | 1:00 | 1:00 |
| 5-9 | 5 | 37 | 1.39 (0.52-3.69) | 0.40 (0.70-2.28) |
| 10-14 | 1 | 25 | 2.11 (0.70-5.59) | 0.52 (0.09-2.99) |
| >15 | 0 | 5 | 1.35 (1.06–1.73)* | 1.04 (0.17-6.49) |
| Days from symptom onset to intubation | ||||
| <5 | 5 | 11 | 1:00 | 1:00 |
| 5-9 | 1 | 29 | 1.26 (0.58- 2.70) | 1.38 (0.58-3.33) |
| 10-14 | 1 | 32 | 2.87 (1.21-6.82) | 3.38 (0.27-8.98) |
| 15-19 | 0 | 11 | 2.96 (0.85-10.30) | 2.79 (0.17-10.87) |
| >20 | 5 | 9 | 1.67 (1.16– 2.42)*** | 1.21 (0.55-2.68) |
| Septic shock | ||||
| yes | 1 | 56 | 17.11 (2.12- 38.27)** | 12.83 (1.46- 13.11)** |
| No | 11 | 36 | 1:00 | 1:00 |
| AKI | ||||
| yes | 2 | 56 | 7.78 (1.61-7.56)* | 2.78 (0.61-10.77) |
| No | 10 | 36 | 1:00 | 1:00 |
| Vasopressors | ||||
| yes | 1 | 59 | 0.05 (0.006-0.41)* | 1.08 (0.47-17.56) |
| No | 11 | 33 | 1:00 | 1:00 |
| IMV | ||||
| yes | 7 | 86 | 10.24 (2.48-4.14)** | 5.28 (1.01–7.71)*** |
| No | 5 | 6 | 1:00 | 1:00 |
NB: *: significant; *p<0.05; **p<0.01 and ***p<0.001
Risk factors for treatment outcomes of mechanically ventilated clients
The results of uni-variate logistic regression analysis found that patients with the complaint of fatigue at presentation (COR=8.5; 95% CI: 2.12-4.03), duration of onset of symptoms to ICU admission and intubation (COR=1.35; 95% CI: 1.06- 1.73 and COR=1.67; 95% CI: 1.16-2.42), respectively, the presence of complication (COR=9.89; 95% CI: 1.73-6.39), septic shock (COR=17.11; 95% CI: 2.12-38.27), AKI (COR=7.78; 95% CI: 1.61-7.56), treatment with vaso-pressors (COR=0.05; 95% CI: 0.006-0.41), those patients who received IMV(COR=10.24; 95% CI: 2.48-4.14) were risk factors associated with the death of patients who were put on MV in the ICU. Furthermore, the forward stepwise multivariate logistic analysis was done by including variables who were significant with missing data <30% and P value < 0.05 in the uni-variate analysis and also by avoiding variables with strong correlation in the analysis. In the final model three out of five predictor variables were found to be statistically significant, this include fatigue(AOR=7.59 ; 95% CI: 1.65-5.12), IMV (AOR=5.28; 95% CI: 1.01-7.71) and septic shock (AOR=12.83; 95% CI: 1.46-13.11) were a significant risk factors for the ICU mortality of the patients (Table 5).
Discussion
The study was done on 104 patients with confirmed SARSCoV-2 infection, accounting for the overall 29% ICU admission of hospitalization of which about 63% of patients received mechanical ventilation among the study groups. However, the studies done in Germany (74%), Spain and Andorran hospital (64.6%) and Italy (97.7%) on patients who received ventilatory support reported higher prevalence of use of MV [17,27,28-31]. The explanation for this may be because of higher prevalence of the cases in the western country at the time of the study those requiring ICU level of care and older age patients prevalence with co-morbidity. However, the result found higher percentage than the study done in Pakistan (9%) and Morocco (48.9%) this is may be due to the enrolment of lower number of study population and lower prevalence of the cases in the country at the time of the study and in Africa in general [32-34].
At the study’s cutoff date of the entire cohort, 165(14.6%) were admitted to the intensive care unit with the overall ICU mortality of 61.8%. Among the 104 patients who received mechanical ventilation, 92(88.5%) died, 12(11.5%) were discharged from ICU. This finding of mortality of patients is higher despite the low rate of ICU admission and overall mortality than studies done in Spain (32%) [27), Germany (44%) [17], Morocco (31.1%) [34], Wuhan China (43%) [29], and also Italy 48.7% death with discharge in 51.4% of patients (28). This finding is comparable to studies done in developing countries including Tunisia 70% death and 30% discharge [35], Kuwait 59.49% ICU deaths and Pakistan (75%) [32], This is may be due to delayed access to high care units/ICU, shortage of critical care resources, inadequate skill sets of treatment provider, severe disease at presentation and referral of severe cases from different facilities, prevalence of comorbidity, difference in management and not following treatment guidelines are some of the reason that can be mentioned.
The rate of NIV therapy failure in our study was 65.5% which was lower than the study done in Germany hospital which was about 74% [17]. The explanation for this may be because of higher utilization of NIV at initial admission of patients to the ICU in Germany hospitals as first line of management than in our setting and also may be because of lower utilization of NIV for the risk of nosocomial acquiring of COVID to the heath-care personnel due to inadequate availability of PPE, in addition difference in the setting of the ICU standards which help in reducing the risk of exposure. This finding was also supported by the low use of IMV and higher use on NIV in the studies done in USA, southeast Mexico and Italy than in our study [23,24,25,28]
Our study found that According to disease severity majority 56(53.8%) of patients were severe cases, 26% moderate and 19.6% were mild cases at the time of triage at the treatment center. This finding has shown difference with study done in Germany, Spain, and Tunisia [17,27,35]. The finding is may be because of the high referral rate of severally ill patients to our hospital for better management of complicated cases which majority of them requiring more advanced care in ICU that are not available in other hospitals as it serves as a major referral center.
In this study the major top three comorbidity among our patients were Hypertension (64.2%), Diabetic mellitus (38.3%), and 18.5% (CKD). This is in agreement with studies from USA, Spain, Oman and Morocco [23,24,27,33,34]. In this study about 36.5% of our study population has at least one major comorbidity this percentage is much lower than in studies done in Germany (69%), Southeast Mexico (72 %), Italy (60.3%), Wuhan (51%), and Morocco (73.3%) [17,25,28,29,34].
In terms of initial presenting symptoms of patients to the hospital our study found that the most common complaints were SOB (85.9%), fatigue (71.70%), dry cough (67.7%), and fever (56.6%). This result is similar to studies done in Kuwait, Mexico, China in Wuhan city, Morocco, and Tunisia [15,25,30,34,35].
In our cohort study, we observed the median duration from onset of symptoms to ICU admission for patients who presented to the hospital was 8 [5,10] days. This finding was somehow lower than studies done in Italy with median days of 10 [6-14], and in Tunisia 11.3±1.2 [28,35]. Median duration from onset of symptoms to intubation for patients who presented to the hospital was 10 [6-12] which was lower than the finding in Mexico 11 [6-14] and Spain 12 [9-16] [26,27]. This is may be due to higher rate of critical patients presenting to the hospital and lower prevalence of utilization of NIV. For the study done in morocco shows shorten duration of patients presentation to ICU admission which is about 3(2-7) [34]. This is may be due to the small number of the study sample as compare to our study.
This study reported that the median age of patients that were admitted to ICU and received ventilatory support was 60 (IQR; 45-70) and mean of 56.96(±17.2) with 58.7% of patients being ≤64 years this result is in line with results done in the African continent [34,35]. But this finding has lower older age group as compared to studies done in Germany, USA, and Spain [17,24,25,27]. This is maybe due to higher older age group in the western population and also as its shown in there study population.
With respect to laboratory results the study showed higher prevalence of lymphopenia (79.6%), leukocytosis (56.7%), neutrophilia (63.6%), normal platelet count (63.1%), normal hematocrit (54.1%), high AST (74.7%), high ALT (74.7%), high urea and creatinine in 61.8% and 38.2% respectively, normal total bilirubin in 95.5%, hyperglycemia in 74.6%. This result is line with study done on systemic review and meta-analysis of in 7 countries which include 28 different studies [31] and in Wuhancity of china [30]. In our study the result of RFT was higher than study done in Oman [33] this explained by higher prevalence of AKI in our study.
The research has found that the majority of treatments received in our hospital were steroid (100%), antibiotic (99%), therapeutic anticoagulation (70.2%), vasopressors (57.7%) and also RRT (17.3%). In this study only 12(11.5%) received neuromuscular blockade and 1% of patients received experimental therapy. However, this result has shown major difference in terms of management of patients with respect to studies done in Germany, Morocco, and Tunisia [17,35,34). This difference is may be due to different management protocol implementation between hospitals and countries at the time of the pandemic and also there was no clear known curative therapy for the illness which was proven to be used. So different institutions and county was in disparate use of any solution available at hand to curb the worsening of the situation.
The study also found that the three most common complication developed by the patients while on MV in ICU were HAP (68%), AKI (59.8%), and septic shock (58.8%). This result is also in agreement with studies done in and Germany (17%).
Our study found that the median hospital length of stay in ICU for deceased patient was 10 days (IQR, 5-14days), and the mean (SD) was 11.35(±7.19) days. Among patients with an ICU admission on ventilator support, the mean (SD) ICU LOS was estimated to be 8.08(6.24) days, and the median (IQR) was 7 [3- 11] days and also the mean (SD) duration of MV support was estimated to be 6.27(5.92) days, and the median (IQR) was 4.5 [2- 8] days. This result is similar to study done in Tunisia for ICU LOS was 11.2±5.8 [35]. But it was lower than studies done in Wuhan with duration of IMV and ICU LOS 10.12 and 7.78 respectively [29]. Duration of MV and ICU LOS were higher in Germany 15 [8-25] vs. 18 [8-25], Spain 14 [7-24] vs. 19 [11-35] and Italy 10 [6-17] vs. 12 [6-21] days [17,27,28]. The possible explanation for this may be due higher mortality rate of patients which may increase the turn-over of patient admission to in ICU.
Limitation of the study
The identification of some clinical diagnosis was relied on treating physicians not on confirmatory diagnosis, so these may leaded to over diagnosis of some cases.
We may have included disproportionately more patients with poor outcomes (due to the transfer of patients in serious condition to our hospital).
Due to the retrospective study design, some cases had incomplete documentation of laboratory testing and other important parameters.
Conclusion
In this single-center retrospective observational study of patients, severe acute complications were common. Death disproportionately affected older between the age of 65-79 years and male patients.
Rate of ICU admission was 29% at the time of the study and among these 104 patients required mechanical ventilator support. Among the total study patients 11(10.6%) patients received only non-invasive ventilation. 21(20.2%) patients were treated with non-invasive ventilation prior to endotracheal intubation. Thus, 93 patients (89.4%) over all received invasive mechanical ventilation
At the end of the study period about 12(11.5%) patients were discharged from ICU and 92(88.5%) patients were died in the ICU with the overall ICU mortality of 61.8% among 165 patients admitted in the ICU including those who did not received mechanical ventilation.
The results of uni-variate logistic regression analysis found that patients with the complaint of fatigue at presentation, duration of onset of symptoms to ICU admission and intubation respectively, the presence of complication, septic shock, treatment with vasopressors, those patients who received IMV were risk factors associated with the death of patients who were put on MV in the ICU. Furthermore, the forward stepwise multivariate logistic analysis was done in the final model three out of five predictor variables were found to be statistically significant, this include fatigue, IMV and septic shock were a significant risk factors for the ICU mortality of the patients.
Recommendation
Based on our finding early use of NIV should be practiced early as much as possible and delayed practice of IMV should be avoided.
Prioritizing of patients on use of available resource based on possible outcome should be considered
For practicing physicians should improve on proper documentation of patients data and finding and also they have follow protocols written for COVID management as much as possible
For the minister of health bureau: the bureau should continuously advocate and work on prevention the disease by involving different stake holders and address the low coverage of vaccination especially for those vulnerable groups of patients.
For SPHMMC: the institution should try to solve the issues related to patients chart keeping and proper documentation by using electronic method of record keeping to solve the discrepancies created at different level and should try to follow specific protocols in the management of the patients in COVID ICU.
Declarations
Ethical approval and consent to participate: The research proposal was approved by the ethical review board of St. Paul’s hospital millennium medical college. A formal letter of permission and support was written to ICU department. Informed consent was obtained from all subjects.
This study was done on secondary data from patient charts. The data from the case records was handled with strong confidentiality. The study was started after ethical clearance was obtained from the review board and after permission from the hospital management to review records.
Consent for publication: Informed consent was obtained from all subjects.
Availability of data and materials: Data and materials are available and can be shared by the corresponding author.
Competing interests: There is no competing interest among the authors.
Funding: No fund was obtained for this study.
Acknowledgment: We acknowledge the SPHMMC/EMCC department .
References
- Tyrrell DAJ, Myint SH. Coronaviruses. In: Baron S, editor. Medical Microbiology. Galveston (TX): University of Texas Medical Branch at Galveston Copyright ©. The University of Texas Medical Branch at Galveston. 1996.
- Cong Y, Verlhac P, Reggiori F. The Interaction between Nidovirales and Autophagy Components. Viruses. 2017; 9: 182.
- Acuti Martellucci C, Flacco ME, Cappadona R, Bravi F, Mantovani L, et al. SARS-CoV-2 pandemic: An overview. Advances in biological regulation. 2020; 77: 100736.
- McIntosh K, Becker WB, Chanock RM. Growth in suckling-mouse brain of “IBV-like” viruses from patients with upper respiratory tract disease. Proceedings of the National Academy of Sciences. 1967; 58: 2268-73.
- Hozhabri H, Piceci Sparascio F, Sohrabi H, Mousavifar L, Roy R, et al. The Global Emergency of Novel Coronavirus (SARS-CoV-2): An Update of the Current Status and Forecasting. International journal of environmental research and public health. 2020; 17.
- Woo PCY, Huang Y, Lau SKP, Yuen KY. Coronavirus Genomics and Bioinformatics Analysis. Viruses. 2010; 2: 1804-20.
- Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta bio-medica: Atenei Parmensis. 2020; 91: 157-60.
- Zhu N, Zhang D, Wang W, Li X, Yang B, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. New England Journal of Medicine. 2020; 382: 727-33.
- Kebede Y, Yitayih Y, Birhanu Z, Mekonen S, Ambelu A. Knowledge, perceptions and preventive practices towards COVID-19 early in the outbreak among Jimma university medical center visitors, Southwest Ethiopia. PloS one. 2020; 15: e0233744.
- Cheng VCC, Lau SKP, Woo PCY, Yuen KY. Severe Acute Respiratory Syndrome Coronavirus as an Agent of Emerging and Reemerging Infection. Clinical Microbiology Reviews. 2007; 20: 660-94.
- Hui DS, I Azhar E, Madani TA, Ntoumi F, Kock R, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health — the latest 2019 novel coronavirus outbreak in Wuhan, China. International Journal of Infectious Diseases. 2020; 91: 264-6.
- Liu W, Tao ZW, Wang L, Yuan ML, Liu K, et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chinese medical journal. 2020; 133: 1032-8.
- Mungroo MR, Khan NA, Siddiqui R. The increasing importance of the novel Coronavirus. Hospital Practice. 2021; 49: 1-11.
- Singhal T. A Review of Coronavirus Disease-2019 (COVID-19). The Indian Journal of Pediatrics. 2020; 87: 281-6.
- Ayed M, Borahmah AA, Yazdani A, Sultan A, Mossad A, et al. Assessment of clinical characteristics and mortality-associated factors in COVID-19 Critical cases in Kuwait. Medical Principles and Practice. 2020.
- Anjorin AA, Abioye AI, Asowata OE, Soipe A, Kazeem MI, et al. Comorbidities and the COVID-19 pandemic dynamics in Africa. Tropical medicine & international health: TM & IH. 2021; 26: 2-13.
- Roedl K, Jarczak D, Thasler L, Bachmann M, Schulte F, et al. Mechanical ventilation and mortality among 223 critically ill patients with coronavirus disease 2019: A multicentric study in Germany. Australian critical care: official journal of the Confederation of Australian Critical Care Nurses. 2020; 34: 167-75.
- Murthy S, Leligdowicz A, Adhikari NK. Intensive care unit capacity in low-income countries: a systematic review. PloS one. 2015; 10: e0116949.
- Wu C, Chen X, Cai Y, Xia J, Zhou X, et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020; 180: 934-43.
- Angriman F, Scales DC. Estimating the Case Fatality Risk of COVID-19 among Mechanically Ventilated Patients. American journal of respiratory and critical care medicine. 2021; 203: 3-4.
- Kirenga B, Muttamba W, Kayongo A, Nsereko C, Siddharthan T, et al. Characteristics and outcomes of admitted patients infected with SARS-CoV-2 in Uganda. BMJ open respiratory research. 2020; 7.
- Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020; 323: 2052-9.
- Auld SC, Caridi-Scheible M, Blum JM, Robichaux C, Kraft C, et al. ICU and Ventilator Mortality Among Critically Ill Adults With Coronavirus Disease 2019. Critical care medicine. 2020; 48: e799-e804.
- Cedano J, Fabian Corona E, Gonzalez-Lara M, Santana M, Younes I, et al. Characteristics and outcomes of patients with COVID-19 in an intensive care unit of a community hospital; retrospective cohort study. Journal of community hospital internal medicine perspectives. 2021; 11: 27-32.
- Ñamendys-Silva SA, Alvarado-Ávila PE, Domínguez-Cherit G, Rivero-Sigarroa E, Sánchez-Hurtado LA, et al. Outcomes of patients with COVID-19 in the intensive care unit in Mexico: A multicenter observational study. Heart & Lung. 2021; 50: 28-32.
- Cortés-Tellés A, López-Romero S, Mancilla-Ceballos R, OrtízFarías DL, Núñez-Caamal N, et al. Risk Factors for Mortality in Hospitalized Patients with COVID-19: An Overview in a Mexican Population. Tuberculosis and respiratory diseases. 2020; 83: S46-s54.
- Ferrando C, Suarez-Sipmann F, Mellado-Artigas R, Hernández M, Gea A, et al. Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive care medicine. 2020; 46: 2200-11.
- Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA internal medicine. 2020; 180: 1345-55.
- Hua J, Qian C, Luo Z, Li Q, Wang F. Invasive mechanical ventilation in COVID-19 patient management: the experience with 469 patients in Wuhan. Critical care (London, England). 2020; 24: 348.
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet (London, England). 2020; 395: 507-13.
- Chang R, Elhusseiny KM, Yeh YC, Sun WZ. COVID-19 ICU and mechanical ventilation patient characteristics and outcomesA systematic review and meta-analysis. PloS one. 2021; 16: e0246318.
- Ayaz A, Arshad A, Malik H, Ali H, Hussain E, et al. Risk factors for intensive care unit admission and mortality in hospitalized COVID-19 patients. Acute and critical care. 2020; 35: 249-54.
- Khamis F, Al-Zakwani I, Al Naamani H, Al Lawati S, Pandak N, et al. Clinical characteristics and outcomes of the first 63 adult patients hospitalized with COVID-19: An experience from Oman. Journal of infection and public health. 2020; 13: 906-13.
- El Aidaoui K, Haoudar A, Khalis M, Kantri A, Ziati J, et al. Predictors of Severity in Covid-19 Patients in Casablanca, Morocco. Cureus. 2020; 12: e10716.
- Saida IB, Ennouri E, Nachi R, Meddeb K, Mahmoud J, et al. Very severe COVID-19 in the critically ill in Tunisia. The Pan African medical journal. 2020; 35: 136