SciBase Journals
SciBase Critical Care and Emergency Medicine
ISSN 2691-7785
- Article Type: Case Report
- Volume 1, Issue 1
- Received: Nov 16, 2023
- Accepted: Dec 20, 2023
- Published Online: Dec 27, 2023
Hypoganglionosis and Isolated Crohn’s Disease of the Terminal Ileum Presenting with Perforation Mimicking Appendicular Mass in a 72-Year-Old Asian Lady
Devkumar Jitendra Govani1; Miss Indre Zaparackaite2; Shailinder Jit Singh3; Debashish Bhattacharya4; Swamy KB5;Rafael Cavalcante Correia6; Partap Kumar Midha7; Ramnik V Patel8*
1Medical Student, BJ Med College and New Civil Hosp, Ahmedabad, Gujarat, India.
2Department of Pediatric Surgery, Emergency’s Children’s Surgery Hospital, Entebbe/ Evelina Children’s Hospital, London.
3Department of Pediatric Surgery, Nottingham University Hospitals, Nottingham, UK.
4Department of Pediatric Surgery, Sultan Qaboos Hospital, Salalah, Sultanate of Oman.
5Lincoln University College, Lincoln University, Kuala Lumpur, Malaysia.
6Holy House of Tatui Gen Hospital, 330 Maneco Pereira Road, Tatui 18273000, Sao Paulo, Brazil.
7J. Watumull Global Hospital & Research Centre, Delwara Road, Mount Abu, Rajasthan, India Affiliated to Medical Faculty of God Fatherly World Spiritual University, Mount Abu, Rajasthan.
8Departments of Pediatrics and Pediatric Surgery, Postgraduate Institute of Child Health & Research and KT Children Govt University Teaching Hospital, Rajkot 360001, Gujarat, India.
*Corresponding Author: Ramnik V Patel
Department of Pediatric Surgery, Postgraduate Institute of Child Health and Research and KT Children Government University Teaching Hospital, Rajkot 360005, Gujarat India.
Tel: 0044-7956896641;
Email: ramnik@doctors.org.uk
Abstract
A very unusual and interesting case of a 72-year-old Indian female with a background of chronic constipation since early infancy presented in emergency critical condition with acute perforative peritonitis and right lower quadrant fullness, guarding and tenderness. Laboratory studies showed high inflammatory markers and provisional diagnosis of walled off appendicular perforation was made. Radiographs and multi scanner computed tomography (MSCT) was found to have pneumoperitoneum secondary to the terminal ileal stricture with perforation. The patient underwent emergency exploratory laparotomy following initial resuscitation, resection and anastomosis of the ileal stricture, peritoneal toilet and extramucosal biopsies of rectosigmoid colon were performed. Histopathology confirmed isolated Crohn’s disease of terminal ileum with stricture and associated hypoganglionosis. Subsequent colonoscopy and biopsies showed no active Crohn’s disease but had nonspecific colitis of the left colon due to associated hypoganglionosis. The postoperative period was uneventful. The patient is doing well at follow up with conservative management of the hypoganglionosis with laxatives, dietary changes, life style modifications and dietary supplements.
Keywords: COVID-19; SARS-CoV-2; Risk factors; Mortality; Mechanical ventilation.
Citation: Govani DJ, Zaparackaite MI, Singh SJ, Bhattacharya D, Swamy KB, et al. Hypoganglionosis and Isolated Crohn’s Disease of the Terminal Ileum Presenting with Perforation Mimicking Appendicular Mass in a 72-Year-Old Asian Lady. SciBase Crit Care Emerg Med. 2023; 1(1): 1002.
Introduction
Crohn’s disease, a complex transmural chronic inflammatory disease, may involve any part of alimentary tract, commonly occurring in the ileocecal area [1]. The incidence is increasing worldwide. The isolated involvement of the terminal ileum with an initial acute presentation with perforation and associated with hypoganglionosis is a district rarity especially in older patient [2-5]. In this case report, we present a 72 years old female with isolated terminal ileum Crohn’s disease mimicking walled off appendicular perforation. Free perforation of the intestine as first clinical presentation of Crohn’s disease is rare with an incidence of 3.4%, with 86.1% of perforations involving the ileum.
Case report
A 72 years old female patient who had chronic constipation since early infancy but otherwise apparently healthy presented with sudden central abdominal pain shifting to right lower quadrant, nausea, vomiting, high grade fever, abdominal distention and blood in the loose stool. Patient had history of ongoing partial functional large bowel obstruction due to chronic long term constipation being treated conservatively.
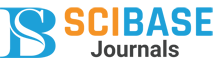
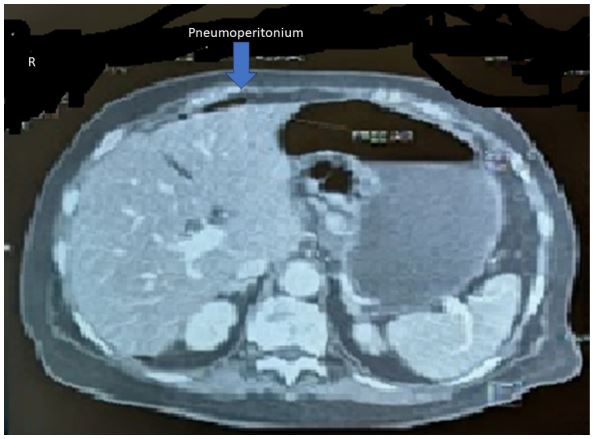
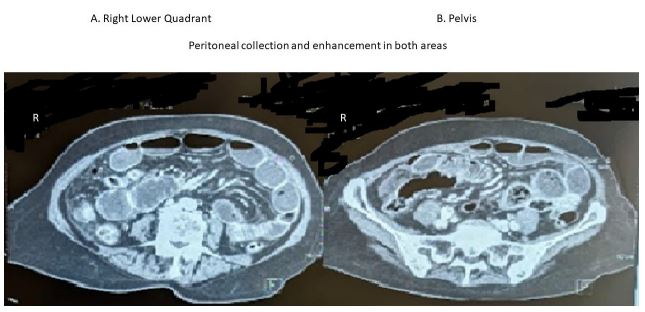
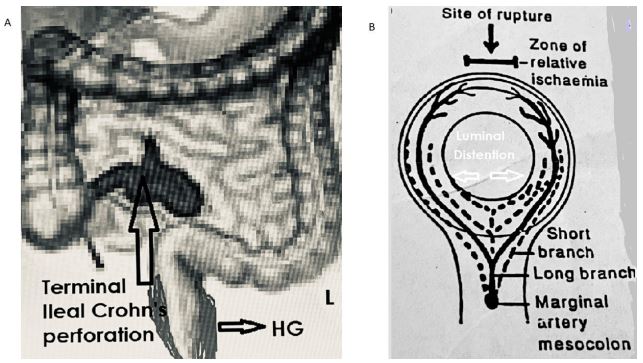
Physical examination revealed pale, listless, febrile with temperature 38.8°C, thready low volume pulse 126/min, blood pressure of 88/56 mm Hg, central capillary refill of 4.5 min and respiratory rate of 20/min. Abdomen was distended with tenderness, guarding and fullness over right lower quadrant. Rectal examination showed loaded rectum with overflow loose stools and tinge of blood. Laboratory investigations showed hemoglobin 85 g/l, white cell count of 28500 and CRP of 360 g/L. Plain supine abdominal and upright chest radiographs showed pneumoperitoneum suggestive of perforative pathology. Imaging with MSCT scan of abdomen & pelvis confirmed the presence of pneumoperitoneum (Figure 1). There was mucosal enhancement and peritoneal collection in the right lower abdomen and pelvic cavity (Figure 2). Mild circumferential wall thickening involving terminal ileum & ileocecal junction with mucosal hyperenhancement, proximal ileal dilation filled with faeces and significant luminal narrowing of ileocecal junction with mesenteric fat stranding was seen (Figure 3).
The patient underwent emergency exploratory laparotomy following initial resuscitation. At exploration, free air escaped on opening the peritoneum, 300-400 ml purulent fluid drained out and a short 2 cm long and 6 mm thick terminal ileal isolated stricture leading to dilation of proximal ileum with an antimesenteric perforation and peritoneal collection together with dilated rectosigmoid with reversed rectosigmoid ratio and severe fecal loading of the left colon was observed (Figure 4A). A thorough peritoneal toilet using copious amounts of warm saline was carried out. Resection of the short segment of the terminal ileum together with the perforated proximal dilated segment and end to end ileoileal anastomosis and extramucosal biopsies of rectosigmoid colon concluded the procedure. Post operative period was uneventful and she recovered well.
Histopathological examination showed focal thickening and transmural chronic inflammation with occasional non caseating granuloma with predominant fibrosis of submucosa & subserosa with isolated single stricture formation and associated perforation measuring 3.5 cm segment. Haphazard crypt organization, ulceration of mucosa and reactive changes in isolated lymph nodes were noted. The findings were suggestive of Crohn’s disease.
Subsequently at the follow up, the patient underwent colonoscopy with biopsies which showed no evidence of any Crohn’s disease but nonspecific retention colitis in the severely loaded left colon maximum being in the rectosigmoid area. The patient is doing well at follow up with anti-inflammatory drug e.g. mesalazine (Pentasa®) and conservative management of the hypoganglionosis with laxatives, dietary changes, life style modifications and dietary supplements.
Discussion
Crohn’s disease, one of the two common inflammatory bowel diseases (IBD), represents a complex interplay of genetic, environmental, and immunologic factors that manifest as chronic inflammation within the gastrointestinal tract. As a clinician immersed in the world of medicine and dedicated to the pursuit of knowledge, the opportunity to present this case report adds a valuable contribution to the ongoing discourse surrounding the diagnosis, management, and understanding of Crohn’s disease and its association with hypoganglionosis with its implications on dysbiosis and altered microbiome and immune consequences.
In this overview of Crohn’s disease, emphasizing its multifaceted etiology, clinical heterogeneity, and the imperative need for comprehensive management strategies by delving into the etio-pathogenesis, clinical presentation, diagnostic modalities, and therapeutic interventions, we aim to contribute to the broader understanding of Crohn’s disease and implications of the associated hypoganglionosis while shedding light on the intricacies of its manifestation in our specific patient case.
Etiopathogenesis depends on various factors like genetic susceptibility, environmental, Immune system, and host microbiome changes [6]. Many genes are involved in pathogenesis of Crohn’s disease. But genes like ATG16L1 and IRGM, both of which are involved in autophagosome formation. Long term use of wide spectrum antibiotics may disturb host microbiota. Our patient presented with severe abdominal pain and acute symptoms and had no protracted chronic symptoms due to very localised and nearly burnt-out disease. As Crohn’s disease is mimicker of acute appendicitis, Crohn’s disease should be suspected in patients who present with an unusual clinical course. fibrofatty proliferation along the mesenteric side of the bowel wall. Fistulas and abscesses may form.
The pathophysiology of antimesenteric perforation in our case can be explained by the fact that isolated terminal ileal stricture development has caused chronic distention of ileum immediate proximal to the stricture. Marginal artery of the colon gives long and short terminal branches to the and their anastomoses across the antimesenteric are meagre, constituting a zone of relative ischemia, making this site of perforation during massive distention and associated inflammation at the borders of the Payer’s patches [7,8]. Most likely site for perforation would be where the anastomoses of the marginal artery are least effective (Figure 4B).
In a localised terminal ileal pathology, we prefer to do localised resection rather than ileocecal resection or hemicolectomy as in Crohn’s disease the surgery needs to be reserved for least invasive option and preservation of terminal ileum and ileocecal valve has so many advantages [9]. The hypoganglionosis is a seen mainly in children and young adults [10-12]. It has been reported in adults but it is rare to see in elderly patients [13]. This can lead to chronic fecal retention leading to dysbiosis of colon, intermittent or continuous ileocecal reflux, small bowel bacterial overgrowth with activation of the immune system network via Payer’s patches and causing malabsorption with multiple micronutrient deficiency [14,15].
Our hypothesis is that in our case perhaps the hypoganglionosis has been a risk factor in predisposition of the inflammatory bowel disease at a later stage by chronic alteration of the microbiome of the hind gut causing dysbiosis initially followed by midgut via ileocecal reflux and small bowel bacterial growth secondarily and tertiarily via feco-oral route altering oral and foregut microbiome which has been implicated in the development of Crohn’s disease recently.
Conclusion
Crohn’s disease is a complex disorder with a wide range of clinical gastrointestinal and extraintestinal clinical features. Understanding differential diagnosis from acute appendicitis and other conditions are crucial to provide accurate diagnosis, appropriate treatment to decrease flare up in Crohn’s disease. Relationship of hypoganglionosis and Crohn’s disease needs to be explored.
References
- Tadesse R, Ewnte B, Tesfaye K. Perforated ileum as the initial presentation of Crohn’s disease, a case report. Int J Surg Case Rep. 2022; 97: 107305. doi: 10.1016/j.ijscr.2022.107305. Epub 2022 Jun 14. PMID: 35907295; PMCID: PMC9403019.
- Jia Hui Lee, Tze Tong Tey, Fung Joon Foo, Frederick Koh, Perforated viscus as first presentation of Crohn’s disease: a case report, Journal of Surgical Case Reports. 2021; 9: 2021: 415. https://doi.org/10.1093/jscr/rjab41.
- Francisco T-E, David M-D, Omar P-B, Rodrigo E-D, Alejandra Z-O. Crohn’s Disease Manifesting as Acute Appendicitis: Case Report and Review of the Literature. World J Surg Surgical Res. 2020; 3: 1185.
- Gnanaselvam P, Weerakoon DN, Wijayasuriya WAM, Mohottala VS, Sinhakumara BMES, Jayarajah U, Banagala ASK. Isolated Crohn’s Disease of the Appendix Presenting as Acute Appendicitis in a 60-Year-Old South Asian Female: A Case Report, Review of Literature, and Follow-Up Recommendations. Case Rep Surg. 2019; 2019: 5285417. doi: 10.1155/2019/5285417. PMID: 31737400; PMCID: PMC6815536.
- Han H, Kim H, Rehman A, Jang SM, Paik SS. Appendiceal Crohn’s disease clinically presenting as acute appendicitis. World Journal of Clinical Cases. 2014; 2(12): 888-892. doi: 10.12998/wjcc.v2.i12.888.
- Petagna L, Antonelli A, Ganini C, Bellato V, Campanelli M, Divizia A, Efrati C, Franceschilli M, Guida AM, Ingallinella S, Montagnese F, Sensi B, Siragusa L, Sica GS. Pathophysiology of Crohn’s disease inflammation and recurrence. Biol Direct. 2020; 15(1): 23. doi: 10.1186/s13062-020-00280-5. PMID: 33160400; PMCID: PMC7648997.
- Yadav K, Mehta M, Endeley EM, Patel RV. Transanal and intraperitoneal prolapse in intussusception. J Paediatr Child Health. 1990; 26(2): 99-100. doi: 10.1111/j.1440-1754.1990.tb02396.x. PMID: 2361074.
- Mehta MH, Patel RV: Intussusception & intestinal perforations caused by multiple trichobezoars. J Pediatr Surg. 1992; 27(9): 1234-1235.
- Govani DR, Patel RR, Patel RV, Doshi S. Ileo-cecal Sphincteric Duplication-Total Cyst Excision with Ileo-cecal Valve Preservation. Austin J Clin Case Rep. 2014; 1(8): 2.
- Govani DJ, Trambadia, RA, Chhaniara RA, Mirani ZR, Chhaniara AP, Midha PK, Swamy KB, Patel RV. Pre-Operative Diagnosis of Infantile Triad of Waugh’s Syndrome Associated with-Hypoganglionosis-Key Radiological Findings. Health Child Pediatr SMP. 2023; 1: 1-9.
- Govani DJ, Govani ND, Govani DR, Panchasara NG, Patel RR, Midha PK, Correia RC, Patel RV. Successful Conservative Management of Triple Pelvic Outlet Functional Obstruction Syndrome with Voiding, Menstrual and Bowel Dysfunctions in an Adolescent Girl with long term follow up. J Urol Neph St. 2023; 4(2): 425-31. JUNS.MS.ID.000181. DOI: 10.32474/JUNS.2023.04.000181.
- Govani DJ, Govani ND, Govani DR, Panchasara NG, Patel RR, Midha PK, Correia RC, Patel RI. Successful Conservative Management of Dysfunctional Elimination Syndrome Associated with Micronutrient Deficiencies, Recurrent Juvenile Allergic Urethritis and Penoscrotal Edema. Med Discoveries. 2023; 2(1): 1018.
- Detroja PL, Trambadia RA, Chhaniara RA, Mirani ZR, Midha PK, Patel RV. Mini-series of variety of giant renal calculi as sociated with pelviureteric junction obstruction and hypoganglionosis. Open J Clin Med Images. 2023; 3(1): 1095.
- Zaparackaite I, Singh SJ, Bhattacharya D, Kansagra PJ, Swamy KB, Correia RC, Midha PK, Patel RV: Exploring the characteristics of gut microbiome in patients of Southern Fujian with hypocitraturia urolithiasis and constructing clinical diagnostic models. Int Urol Nephrol. 55, 1917-1929.” by Wang et al. Int Urol Nephrol 55-Manuscript - UROL-D-23-01558.
- Govani DJ, Trambadia RA, Chhaniara RA, Mirani ZR, Midha PK, Correia RC, Patel RV. “Is anemia frequently recognized in gastroschisis compared to omphalocele? A multicenter retrospective study in southern Japan” by Sugita, K et al. Pediatr Surg Int. 2022; 39(1): 26. doi: 10.1007/s00383-022-05288-8. PMID: 36454276.