SciBase Journals
SciBase Critical Care and Emergency Medicine
ISSN 2691-7785
- Article Type: Short Report
- Volume 2, Issue 1
- Received: Mar 08, 2024
- Accepted: April 17, 2024
- Published Online: April 24, 2024
Rare Complication of Fournie’s gangrene following Alcohol Sclerotherapy for Hydrocele: A Case Report
José Cherem1; João Pedro de Sá Pereira2; Laryssa Chaves Vieira2; Joziana Muniz de Paiva Barçante1*
1Biomedical Research Center at the Federal University of Lavras (NUPEB/UFL), Brazil.
2Medical Student, Federal University of Lavras, Brazil.
*Corresponding Author: de Paiva Barçante JM
Biomedical Research Center at the Federal University of Lavras (NUPEB/UFLA), Brazil.
Email: joziana@ufla.br
Abstract
We present a rare case of an 80-year-old male with a longstanding, asymptomatic right hydrocele seeking repair. Hydrocele, characterized by an abnormal accumulation of serous fluid between the parietal and visceral layers of the tunica vaginalis, is a common condition affecting adult males. While surgical removal remains the gold standard treatment, alternative non-invasive approaches such as sclerotherapy have been explored due to their reported high success rates ranging from 85% to 96%. In this case, the patient underwent a combination of aspiration (340 mL of fluid) and sclerotherapy using 60 mL of absolute alcohol as the sclerosing agent. Following the sclerotherapy procedure, the patient experienced the development of a scrotal wound within 72 hours, which progressed to a necrotic point with associated hyperemia at 96 hours. Subsequently, the patient presented with an unusual necrosis in the scrotal sac, rapidly progressing to Fournier’s gangrene, requiring surgical debridement three surgical debridements seven days post-procedure, followed by antibiotic therapy and 35 hyperbaric sessions. Remarkably, the patient’s condition progressed painlessly, and complete closure of the necrotic lesion was achieved. However, this case underscores the importance of cautious evaluation when considering alcohol sclerotherapy in elderly patients, despite its minimally invasive nature. It serves as a reminder of the potential complications that can arise from non-surgical approaches for hydrocele management and highlights the need for careful patient selection and follow-up in such cases.
Keywords: Hydrocele; Sclerotherapy; Scrotal necrosis; Alcohol; Elderly patients.
Citation: Cherem J, de Sa Pereira JP, Vieira LC, de Paiva Barçante JM. Rare Complication of Fournie’s gangrene following Alcohol Sclerotherapy for Hydrocele: A Case Report. SciBase Crit Care Emerg Med. 2024; 2(2): 1007.
Introduction
Hydrocele is a common condition characterized by the abnormal accumulation of serous fluid within the tunica vaginalis surrounding the testicle. While surgical removal remains the gold standard treatment, alternative non-invasive approaches have gained attention due to their reported success rates and reduced surgical risks [1-3]. Among these approaches, sclerotherapy has emerged as a minimally invasive option, involving the injection of a sclerosing agent into the tunica vaginalis to promote adhesion and resolution of the hydrocele [1-3]. Herein, we report a rare complication of scrotal necrosis following alcohol sclerotherapy for hydrocele repair in an elderly male patient.
Case presentation
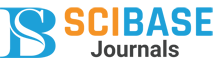
An 80-year-old male presented with a longstanding, asymptomatic right hydrocele, causing aesthetic discomfort due to scrotal enlargement. Given the patient’s advanced age and desire for a minimally invasive approach, a combination of aspiration and alcohol sclerotherapy was performed. Within 72 hours post-procedure, a scrotal wound developed, progressing to necrosis with associated hyperemia at 96 hours (Figures 1A-B). Surgical debridement was subsequently performed, followed by antibiotic therapy and hyperbaric sessions to achieve complete closure of the necrotic lesion (Figures 2A-B).
Discussion
While sclerotherapy is considered a minimally invasive alternative for hydrocele repair, our case highlights the potential risk of severe complications, including scrotal necrosis, particularly in elderly patients. Despite its reported success rates, careful patient selection and monitoring are imperative to minimize adverse outcomes. Clinicians should exercise caution when considering alcohol sclerotherapy, especially in elderly individuals, and remain vigilant for signs of complications post-procedure.
Conclusion
This case underscores the importance of careful patient selection and monitoring when opting for non-surgical approaches such as alcohol sclerotherapy for hydrocele repair, particularly in elderly individuals. While promising, these interventions carry a risk of severe complications, emphasizing the need for cautious evaluation and close follow-up in clinical practice.
References
- Beiko DT, Kim D, Morales A. Aspiration and sclerotherapy versus hydrocelectomy for treatment of hydroceles. Urology. 2003; 61: 708-12.
- Shan CJ, Lucon AM, Arap S. Comparative study of sclerotherapy with phenol and surgical treatment for hydrocele. J Urol. 2003; 169: 1056-9.
- Onol SY, Ilbey YO, Onol FF, Ozbek E, Arslan B, et al. A novel pullthrough technique for the surgical management of idiopathic hydrocele. J Urol. 2009; 181: 1201-5.