SciBase Journals
SciBase Dentistry and Oral Sciences
ISSN 2996-363X
- Article Type: Research Article
- Volume 2, Issue 1
- Received: Jan 17, 2024
- Accepted: Feb 16, 2024
- Published Online: Feb 23, 2024
Raney Clip Free Coronal Scalp Flap: Case Series
Andrew Gayed1*; Timothy Woernley2; Nagi Demian3; Craig Pearl2
1UT Health School of Dentistry, Houston, TX, USA.
2Assistant Professor, Non-Tenure Clinical, UT Health School of Dentistry, Houston, TX, USA.
3Professor & Thomas M. Weil Professorship in Oral and Maxillofacial Surgery, UT Health School of Dentistry, Houston, TX, USA.
*Corresponding Author: Andrew Gayed
UT Health School of Dentistry, Houston, TX, USA.
Tel: 713-397-8782;
Email: Andrewgayed487@gmail.com & Andrew.gayed@uth.tmc.edu
Abstract
The coronal scalp flap is a useful surgical approach that provides access to the upper and middle third of the skull and can be utilized to repair fractures of the upper and middle face. Intraoperative hemostasis is usually achieved with Raney clips. This case series report discusses the literature on the conventional use of Raney clips during coronal flaps elevation and compares it to the technique used by the Oral and Maxillo-facial department at Memorial Hermann Hospital where use of clips are replaced by an electrosurgical cutting and coagulation device, LigaSure. This technique was used by the department on 21 patients treated at MHH. Use of LigaSure was found to decrease intraoperative bleeding as well as reduce alopecia commonly associated with coronal scalp flaps.
Keywords: Craniofacial trauma; Coronal approach; Hemostasis; Alopecia; Case series.
Citation: Gayed A, Woernley T, Demian N, Pearl C. Raney Clip Free Coronal Scalp Flap: Case Series. SciBase Dent Oral Sci. 2024; 2(1): 1009.
Introduction
The coronal scalp flap is a useful approach that provides access to the upper and middle third of the skull and can be utilized to repair fractures of the upper and middle face. This surgical approach has been used by neurosurgeons for over a century [1]. It was originally described in 1907 by Hartley and Kenyon for use in neurosurgical procedures and then adopted by Tessier in craniomaxillofacial surgery in 1970s [1-3]. A coronal flap is a versatile flap used by plastics surgery [4], neurosurgery [5] and oral and maxillofacial surgery [2]. Whether utilized for tumor resections or more recently for facial feminization surgery, the coronal approach provides exposure to the facial architecture with minimal morbidity [2,6]. In Oral and Maxillofacial surgery, this approach is commonly used following trauma, more precisely indicated for fractures of the frontal bone, naso-orbito-ethmoid fractures, comminuted fractures of the zygomatic arch, or when osteotomies are needed for complex midface reconstruction procedures [2,3,7,8].
Though intimidating to novice surgeons, the coronal surgical approach is a safe, reliable and relatively aesthetic procedure which provides an array of possibilities and uniquely exposes the facial skeleton [1-3]. Many incision designs have been proposed in the literature. Thorough dissection through the skin, subcutaneous, galea aponeurotica, loose areolar and periosteum layers (SCALP) is performed [4]. The incision can be unilateral or bilateral and is normally placed within the hairline and extended to the helix of the ears bilaterally. Then anteroposterior position of the incision as well as the lateral preauricular/ postauricular extensions are the main variables of the incision pattern depending on the clinical scenario i.e. male pattern baldness or need to expose the zygomatic arch [1]. The blood supply of interest are mainly the supratrochlear, supraorbital and superficial temporal arteries [4,8]. Intraoperative hemostasis is usually achieved with Raney [5,9].
A Raney clip free technique is used by the Oral and Maxillofacial department at Memorial Hermann Hospital (MHH) and replaced by an electrosurgical cutting and coagulation device, LigaSure. The use of LigaSure was found to decrease bleeding and henceforth improve operative efficiency and overall operative time. This technique was used by the department on 21 patients treated at MHH. The data was collected retrospectively and patient specific information was de-identified. The average patient’s age was 41 years with a mode of 36 years old. Male to female ratio was 13:8.76% of cases were trauma induced, of which motor vehicle crashes alone accounted for 40% of the causative injury. Cerebrovascular events accounted for 19% of cases with equal repartition between ischemic and hemorrhagic events. Patients averaged an ASA of 3 and were smoker or former smokers in 52% of the time.
Surgical technique
Multiple incision designs have been described, from zig zag to straight line to aid in scar camouflage. The author prefers a curvilinear design with the first curve from the lateral extent of incision caudad. This decreases the risk of damage to superficial temporal artery. A curvilinear incision is drawn from helix to helix with the first curve from helix starting caudad (Figures 1 and 2). When access to the zygomatic arch is needed, the author then elects for a lateral extension of the skin incision to include the preauricular region [8]. The incision line is then infiltrated with 1% lidocaine with 1:100,000 epinephrine in the subgaleal plane. This aids in hemostasis and eases the dissection in the appropriate plane [8]. Classical techniques describe the use of Raney clips at scalp flap edges with bipolar cautery to aid in hemostasis [7,8,10]. There is a concern for the use of cautery over the dermal layer while elevating a coronal scalp flap and the potential damage to hair follicles [8]. Ruiz et al. describe the use of low monopolar cautery below the skin and dermis to minimize blood loss without causing damage to the hair [9]. We follow Ruiz’s recommendations by using a LigaSure cautery for hemostasis and dissection in the dermis region [9].
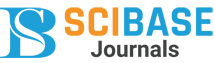
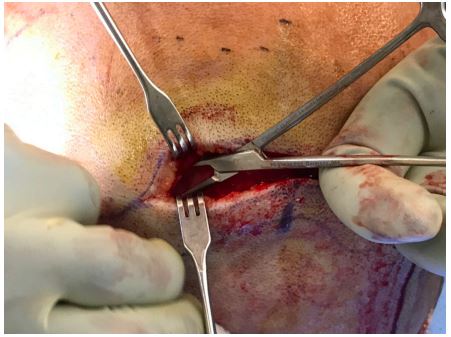
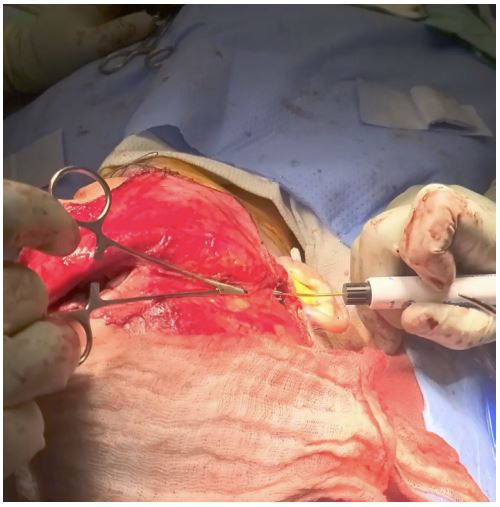
The author places the incision starting at the vertex of the head with a 15-blade through the skin and subcutaneous tissue. The scalp edge is then retracted in an upward fashion with skin hooks and blunt dissection with hemostats is used to identify the pericranium and subgaleal plane (Figure 3). Once the appropriate plane is identified it can be carried along the incision with LigaSure for dissection and hemostasis (Figure 4). Once the entire planned incision is completed and hemostasis achieved, further dissection in the subgaleal can be completed bluntly. The author usually uses finger dissection either with a #9 periosteal or the back end of a blade. This is carried down the forehead to approximately 1.5 cm above the supraorbital rim. At this point an incision is made through the periosteum and subperiosteal dissection is carried further to identify the supraorbital rim and nerve and nasal bones. If an anteriorly based pericranial flap is desired the periosteal incision is made closer to the vertex of the skull and carefully elevated subperiosteally.
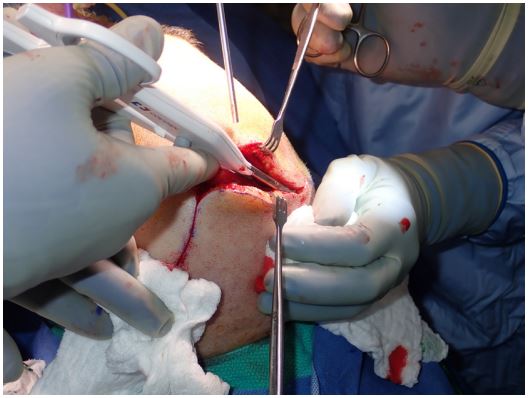
Dissection laterally is determined by need of access such as accesses requiring the degloving of the zygoma. Otherwise, the dissection is limited between the superior temporal lines, then carried down subperiosteally along the lateral orbital wall with little risk to the facial nerve. This allows for further inferior access the nasal bones. For cases that require exposure of the zygomatic arch, preauricular extensions maybe needed (Figure 5). Ruiz et al. advocate for a postauricular approach to avoid damage to the temporal branch of the facial nerve as well as any potential for scaring [9]. Careful dissection over the temporalis muscle is performed to ensure the plane of dissection is deep to the temporal branch. As depicted by Elis and Zide, we prefer to perform the dissection deep to the superficial layer of the temporalis fascia and right above the temporalis muscle and fat [8]. As the dissection proceeds inferiorly, the periosteum can be incised over the zygomatic arches to expose bone (Figure 6).
Discussion
The coronal scalp flap is a useful approach that provides access to the upper and middle third of the skull and can be utilized for repair of maxillofacial trauma. Multiple techniques have been described previously all aiming to provide the required surgical access whilst protecting vital structures and reducing post-operative complications. It is important to underline that in the trained hands, coronal flaps have excellent outcomes with low morbidity [3]. Using a Raney clip free technique further helps eliminate some of the common complications of this approach as previously discussed, alopecia and intraoperative bleeding. Neurological injuries have also been documented. In their 5 years retrospective study, C.J. Kerwala et al. [1] found that the incidence of permanent morbidity was low. Out of 68 flaps included in their study, 35% experienced some form of sensory abnormality immediately after the operation which has resolved in all patients except one within the first 2 years. Frontalis weakness was noted to be the most common complication. In their 271 coronal approaches included in their study, Kleinberger et al. [6] also found similar results with a complication rate of 3.6%. They have further observed a hematoma rate of less than 1%, a scarring and alopecia under 3% and no infections. More importantly, as a result of their modified coronal approach deeper to the temporalis fat pad, none of the cases resulted in either temporary or permanent weakness of the temporal branch of the facial nerve [6]. They stipulate that by following a deeper path of dissection, a greater distance between flap elevation and the course of the frontal branch of the facial nerve and therefore reducing the risk of nerve injury. These results are similar to Singh and Dhungel’s [3] longitudinal prospective study in which similar observations were made. Both authors supported dissection deeper to temporal fat pad reporting no neurosensory or motor deficits.
Blood loss from the coronal incision is greatest at the beginning and end of the surgery [8]. Ellis and Zide described three classical methods to mitigate and reduce blood loss. Initial injection of a vasoconstrictor into the subgaleal plane promotes hemostasis. Running blocking 2-0 sutures polypropylene or nylon along each side of incision line is another measure to reduce intra-operative bleeding. Lastly, special cautery scalpels can be used for scalp incisions to provide hemostasis during incision [8]. The Raney clip free technique used by the Oral and Maxillofacial department at Memorial Hermann Hospital proposes the replacement of the commonly used Raney clips by an electrosurgical cutting and coagulation device, LigaSure.
LigaSure™ Vessel Sealer System (LVSS) was first introduced in 1998 by Valleylab, Boulder, CO, USA. The US Food and Drug Administration [11] has approved the LVSS to seal vessels up to 7 mm in diameter. The seal provided can withstand a minimum of three times normal systolic pressure. The LVSS is designed to deliver a precise amount of energy proportionate to the density of the grasped tissue consequently limiting the much dreaded thermal spread of electrocautery [12]. When compressed between the jaws of the instrument, collagen and elastin fibers in the grasped vessels walls are initially denatured. A cool-down phase is allowed crosslinking reoccurs, effectively creating a new, solid wall of collagen and elastin tissue with the patient own biological tissues [13].
The original intended use of LVSS was aimed at general, laparoscopic, and gynecologic procedures where ligation of vessels was desired and as an alternative to mechanical clamping (clips or staples) or suturing [11]. With increasing hemostatic efficiency and reduction in operative time, it’s use was further expanded to other disciplines and closer to the Oral and Maxillofacial surgery realm in ENT. In the face of increasing data supporting its use, the FDA has further expanded the use of LVSS in ENT procedures in adults (thyroidectomy, radical neck dissection, parotidectomy, and tonsillectomy) for ligation and division of vessels, lymphatics and tissue bundles 2-3 mm away from unintended thermally-sensitive structures such as nerves and parathyroid glands. We use the newer version of LigaSure introduced initially in 2010, LigaSure Small Jaw (LSJ). LSJ was recently the subject of meta-analysis and systematic review by Chen et al. [14], comparing LSJ use in neck dissection vs conventional method. A 29 minutes reduction in operation time was measured and found statistically significant.
Estimated Blood Loss (EBL) is difficult to predict and usually injury and patient specific. Although he found no precise value of EBL, Sheikh [15] found that the blood loss varied considerably depending on the incision method. In his retrospective study over 85 cranial wounds, Sheikh used the number of gauze swabs and the size of blood staining on each gauze piece to compare between electrocautery and scalpel. While no specific numeric were described, he reported that electrocautery scalp incisions averaged four times less compared to the side incised by the steel scalpel. In our experience at MHH, we found that EBL was usually reduced when compared to other services undergoing similar coronal approaches. EBL was measured in all 21 cases performed at MHH and averaged 100 ml. As this procedure was part of a staged surgery, all 21 patients have undergone a second surgery in which the use of Raney clip was applied by a different service and averaged contrastingly 470 ml. Although the nature of the second procedure was different from the first, this 4 fold increase in EBL may be, at least in part, attributed to the use of Raney clips. In Greece, 2007, Vassilios A. Lachanas et al. [12] compared in their prospective study the use of LVSS versus cold knife tonsillectomies in 161 adult patients. Ligasure use lead to no measurable bleeding during surgery in any of the cases compared to 73 +/- 22.11 ml with conventional cold knife technique.
Another advantage of using a Raney clip free technique is lower comparable alopecia [4]. None of the 21 patients treated at MHH developed post-operative alopecia. This is congruent with the recent retrospective study by Kadakia et al. aimed to measure whether post-operative alopecia is more common when bicoronal incisions are performed with monopolar cautery, Colorado microdissection tip cautery, or traditional cold steel and whether this outcome is affected by the use of Raney clips. The study was undergone over 505 patients undergoing bicoronal incisions in a single head and neck surgery practice from 1997 to 2015 with a minimum follow-up of 1 year. In comparing the various methods used, the study concluded that the addition of Raney Clips represented significant increase in alopecia in all instances. Additionally duration of Raney clip use was associated with significantly increased alopecia width [4]. Such results are consistent with Nitta et al. as well as Singh and Dhungel’s who concluded that electrocautery skin incision allowed them to avoid skin edge necrosis or alopecia caused by skin clips [3,5].
It was previously mentioned that the incidence of post-operative alopecia is reduced when avoiding Raney clips and its consequent skin edge necrosis. Other factors influencing post-operative alopecia have also been described however. Male baldness is a general concern when performing a bicoronal approach. In line with current literature, Kadakia’s results concluded that the use of the Colorado tip cautery for skin and subcutaneous incision was associated with the greatest degree of postoperative alopecia [4]. Conversely, Nitta et al. suggest that many of those negative effect of monopolar electrocautery may be avoided with what they call “minimal electrical contact” technique as it results in minimal wound damage, minimal scarring, excellent wound healing, and minimal alopecia [5]. C.J. Kerwala et al. advocate that the pivotal point of the bicoronal flap is its most inferior aspect. They therefore suggest that by extending the incision anteriorly and inferiorly in the preauricular area, the bicoronal incision can be pushed further posteriorly. This occipital incision is what they recommend in patients who are prone to male pattern baldness [1]. A zigzag, or “lazy S” configuration, has also been advocated in textbooks to help hide the scar whenever the hair is wet [7]. Massarelli et al. expended on the concept of zigzag incisions reporting that it provides a very well concealed and pleasing scar. They propose a ∼30-45° beveled incision in a random zigzag pattern within the frontotemporal hairline for all craniomaxillofacial surgeries [17].
In this paper we describe our method used at Houston Memorial Hermann Hospital which was found over multiple cases to provide better perio-operative bleeding. One of the disadvantages of Raney clips is that once removed at the time of closure, the hemostatic benefit they offer no longer exist and the compressed vessels will bleed freely, requiring the surgeon to spend additional time to cauterize and even in some instances ligate or suture the bleeding vessels. By using the LigaSure-assisted technique during dissection and surgical access, the flap is hemostatic all throughout the procedure and less bleeding occurs during closure. Nitta et al. found similar results using electrocautery. They also differed from use of Raney clip and managed to control bleeding only with electrocautery set on coagulation mode. They also concluded that electrocautery skin incision is efficacious, especially for extended operation times, because of little blood loss from the edges of skin incision [5]. Likewise, Sheikh found that blood loss during skin opening was three to five times less when the micro-needle electrocautery scalpel was used [15].
Estimated Blood Loss (EBL) is difficult to predict unless a thorough methodical protocol is incorporated. As such, the inherent nature of a retrospective overview of completed surgical cases without a robust protocol leaves room to a lot of subjectivity when it comes to blood loss estimates. In our study, most patients were neurosurgical patients undergoing craniotomies and underwent staged surgeries. In fact all 21 patients have undergone a second surgery in which the use of Raney clip was applied by a different service. Given the nature of the second procedure was different from the first, it is conceivable that other factors may have influenced the 4 fold decrease in EBL. Further studies may be completed with a succinct protocol to evaluate blood loss with and without Raney clips while comparing identical procedures would provide better evidence.
The use of LigaSure cautery and avoiding Raney clips can increase flap development efficiency, decrease operative time, and minimize blood loss. Also, because the LigaSure is used below the skin and dermis there is no damage to hair follicles resulting in a hidden scar and in fact none of our patients developed alopecia. Post-operative follow-up however was relatively short ranging between 3 and 24 months. Although consistent with the literature as previously described, a longer and consistent follow-up would provide a stronger argument on postoperative alopecia.
Conclusion
The use of LigaSure cautery and avoiding Raney clips can increase flap development efficiency, decrease operative time, minimize blood loss and reduce incidence of post-operative alopecia. Although refuted in previous literature, new growing evidence of relative safety of electrocautery even on dermal layer of the scalp is now documented. Nonetheless, we still avoid use of electrocautery on skin and we propose its use through LigaSure in deeper layers. This avoids all together the theoretical possible damage to hair follicles. It offers safety to the dermal layer while using hemostatic advantage of electrocautery in the deeper layers. This technique has been used by the OMFS department at MHH for over 5 years and we believe that its global adoption and implementation is at par with patient standard of care.
Authorship contributions
Dr Andrew Gayed, DMD, OMFS Resident UT Health Houston:
Conceptualization; Data curation; Formal analysis; Investigation; Validation; Visualization; and Roles/Writing - original draft.
Dr Timothy Woernley, DDS, OMFS Assistant Professor NonTenure Clinical:
Conceptualization; Methodology; Project administration; Supervision; Validation; Visualization; and Writing - review & editing.
Dr Nagi Demian, DDS, MD, Professor and Thomas M. Weil Professorship in Oral and Maxillofacial Surgery:
Conceptualization; Supervision; Validation; and Writing - review & editing.
Dr Craig Pearl, BDS, OMFS Assistant Professor Non-Tenure Clinical
Conceptualization; Supervision; Validation; and Writing - review & editing.
References
- Kerawala CJ, Grime RJ, Stassen LFA, Perry M. The bicoronal flap (craniofacial access): an audit of morbidity and a proposed surgical modification in male pattern baldness. Br J Oral Maxillofac Surg. 2000; 38(5): 441-444. doi: 10.1054/bjom.2000.0315
- Shetty SK, Saikrishna D, Kumaran S. A study on coronal incision for treating zygomatic complex fractures. J Maxillofac Oral Surg. 2009; 8(2): 160-163. doi: 10.1007/s12663-009-0039-2
- Singh AK, Dhungel S. Indications and Complications Associated with Coronal Approach to Upper Midface Fracture. J Coll Med Sci-Nepal. 2019; 15(4): 239-243. doi: 10.3126/jcmsn.v15i4.24933
- Kadakia S, Badhey A, Ashai S, Lee TS, Ducic Y. Alopecia Following Bicoronal Incisions. JAMA Facial Plast Surg. 2017; 19(3): 220-224. doi: 10.1001/jamafacial.2016.1741
- Nitta N, Fukami T, Nozaki K. Electrocautery Skin Incision for Neurosurgery Procedures. Neurol Med Chir. Published online 2011: 4.
- Kleinberger AJ, Jumaily J, Spiegel JH. Safety of Modified Coronal Approach with Dissection Deep to Temporalis Fascia for Facial Nerve Preservation. Otolaryngol Neck Surg. 2015; 152(4): 655-660. doi:10.1177/0194599814567869
- Perry M, Holmes S, eds. Atlas of Operative Maxillofacial Trauma Surgery. Springer London; 2014. doi: 10.1007/978-1-4471-2855-7
- Surgical Approaches to The Facial Skeleton, Second Edition (PDFDrive).pdf.
- Ruiz RL, Pattisapu JV, Costello BJ, Golden B. The Coronal Scalp Flap: Surgical Technique. Atlas Oral Maxillofac Surg Clin. 2010; 18(2): 69-75. doi: 10.1016/j.cxom.2010.08.005
- Haggerty CJ, Laughlin RM. Atlas of Operative Oral and Maxillofacial Surgery. 571.
- Summary Of Safety And Effectiveness Information Valleylab Ligasuretm Vessel Sealing System.
- Lachanas VA, Hajiioannou JK, Karatzias GT, Filios D, Koutsias S, Mourgelas C. Comparison of LigaSure Vessel Sealing System, Harmonic Scalpel, and Cold Knife Tonsillectomy. Otolaryngol Neck Surg. 2007; 137(3): 385-389. doi: 10.1016/j.otohns.2007.05.012
- Li YC, Chao A, Yang LY, et al. Electrothermal bipolar vessel sealing device (LigaSureTM) versus conventional diathermy in laparoscopic myomectomy: A propensity-matched analysis. Wu MP, ed. PLOS ONE. 2018; 13(3): e0193611. doi: 10.1371/journal.pone.0193611
- Chen TY, Hsin LJ, Lin WN, Tsai MS, Tsai YT, Lee YC. LigaSure small jaw versus conventional neck dissection: a systematic review and meta-analysis. J Otolaryngol - Head Neck Surg. 2021; 50(1): 21. doi: 10.1186/s40463-021-00504-2
- Sheikh B. Safety and efficacy of electrocautery scalpel utilization for skin opening in neurosurgery. Br J Neurosurg. 2004; 18(3): 268-272. doi: 10.1080/02688690410001732715
- Waknis PP, Prasad GSV, Wadje S. A Simple Method to Control Bleeding by Stationary Paper Clips as an Alternate to Raney Clips During Coronal Incisions. J Maxillofac Oral Surg. 2013; 12(1): 117-119. doi: 10.1007/s12663-011-0225-x
- Massarelli O, Vaira LA, De Riu G. A new aesthetic pretrichial approach for upper third-facial fractures and pathologies: The Crown incision. J Plast Reconstr Aesthet Surg. 2022; 75(2): 788-796. doi: 10.1016/j.bjps.2021.09.042.