SciBase Journals
SciBase Epidemiology and Public Health
ISSN 2996-4555
- Article Type: Review Article
- Volume 2, Issue 1
- Received: Nov 20, 2023
- Accepted: Jan 31, 2024
- Published Online: Feb 07, 2024
Evidence-Based Practice Approach on Clinical Empathy Skills Among Health Professionals: A Systematic Review Protocol
Suja Kumari S1*; Ajee KL1; KT Moly1; Renjulal Yasodharan2; Rafia Islam1
1Amrita College of Nursing, AMRITA Vishwa Vidyapeetham, Kochi, Kerala, India.
2Manipal College of Nursing, Manipal Academy of Higher Education, Karnataka, India.
*Corresponding Author: Suja Kumari S
Amrita College of Nursing, AMRITA Vishwa Vidyapeetham, Kochi, Kerala, India.
Email: sujaharinair@gmail.com
Abstract
Introduction: Effective educational programs promote and strengthen nursing students’ empathetic skills, contributing to health professionals’ pleasure and emotions of personal accomplishment by offering a sense of excellent personal well-being, quality therapeutic management, and clinical expertise.
Objectives: This review will synthesize the available evidence on the effectiveness of clinical empathy in general practice and clinical empathy skill training among health professionals. Review questions were structured using the PICOT framework.
Inclusion criteria: We will include articles that detail original empirical studies and systematic reviews related to empathy skills among health professionals and the effect of empathy training on clinical empathy skills.
Methods: The databases include the National Library of Medicine, SCOPUS, CENTRAL, MEDLINE, PubMed, EMBASE, and EBSCO. The key methods for facilitating the review will be print and electronic resources. Major medical subject heading (mesh) terms in titles and abstracts will be used in the search. To establish existing literature on the empathy training program, the search will contain the terms “empathy,” “clinical empathy,” and “empathy training” in all fields of the databases. The search strategy will commence from 2023 onward with no language restrictions. A team of independent reviewers will screen the retrieved titles, abstracts, and full-text reports and check the data quality using the John Hopkins EBP model and the literature will be systematically reviewed by following PRISMA Guidelines.
Keywords: Empathy; Clinical empathy; Empathy training; Nursing students.
Citation: Kumari SS, Ajee KL, Moly KT, Yasodharan R, Islam R. Evidence-Based Practice Approach on Clinical Empathy Skills Among Health Professionals: A Systematic Review Protocol. SciBase Epidemiol Public Health. 2024; 2(1): 1015.
Introduction
Clinical results are enhanced when patients are given compassionate, patient-centered care. Competency can be further broken down into empathy, communication, and the capacity to establish a rapport with a patient based on trust. Compassionate patient care demands empathy as a critical ingredient. The ability to empathize is the method by which a doctor can learn as much information as possible about a patient’s condition while also being aware of the patient’s problem [1,2]. Empathy enhances the effectiveness of a patient’s treatment and care [3]. In clinical settings, patient outcomes are influenced by how well doctors and patients interact [4].
Empathy declines during educational and training programs, according to solid evidence. Reviewing the characteristics of empathy among health professionals and teaching clinical empathy skills both require an evidence-based practice approach. Medical students’ attitudes towards patients and their families have been improved by educational interventions, according to several patient-reported studies about compassion and empathy [5]. A continuous program is more important than a single training exercise to foster compassion and empathy, according to a few studies that found that different teaching methods have comparable effects [6].
Relevant training will lead to an improvement in health professionals’ empathic skills, which, in turn, will enable them to understand their patients better, establish positive interpersonal relationships with them, and boost their professional satisfaction [7].
There should be possibilities for doctors and nurses to learn or develop empathetic abilities to comprehend patients’ nonsuperficial feelings and offer beneficial care. To modify behaviours in this way, sustained training sessions are necessary. There is no data on the compassion training of medical students or healthcare workers, despite the literature having some controlled trials on empathy, a precursor to compassion [9].
A quasi-experimental study was conducted using a Knowledge, Simulation, and Sharing (KSS) module related to empathy learning among two hundred and fifty nursing students to assess the effectiveness of empathy in clinical education for nursing students in China. Results showed that at the end of the internship, the experimental groups had significantly higher empathy scores and improved communication skills than the control group [10]. A systematic review of the effectiveness of physician empathy in general practice was published in English between July 1995 and July 2011. After screening the literature using specified selection criteria, 964 original studies were selected; seven were included in this review after applying quality assessment. A good correlation exists between physician empathy and patient satisfaction and a positive relationship with strengthening patient enablement. Empathy lowers patients’ anxiety and distress and delivers significantly better clinical outcomes [11].
Need for the study
Literature reports the effectiveness of clinical empathy in general practice clinical empathy skill training among health professionals. Effective educational programs facilitate and improve nursing students’ empathic skills, providing a sense of excellent personal well-being, quality therapeutic management, and clinical expertise to health professionals’ happiness and feelings of personal accomplishment [12,13].
Objectives and review questions
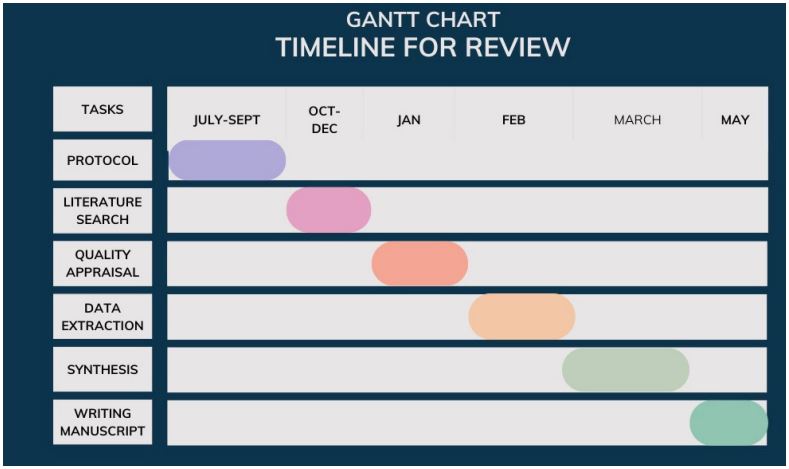
The proposed study aims to systematically review existing literature concerning all studies published in the last 10 years (2012-2022) on the effectiveness of clinical empathy in general practice and clinical empathy skill training among health professionals. Review questions were structured using the PICOT framework. The study will address the following questions.
1. Which characteristics of the featured studies are related to the clinical empathy skills among health care professionals?
2. Does an empathy skill training program improve clinical empathy skills among health professionals?
Methods of the review
Search strategy
Resources from the relevant databases include the National Library of Medicine, SCOPUS, CENTRAL, MEDLINE, PUBMED, EMBASE, and EBSCO. Print and electronic resources will be the primary tools to facilitate the review. The search will use major medical subject heading (MeSH) terms in titles and abstracts. The search will mainly concentrate on studies that detail empathy training among health professionals to improve clinical empathy skills. The search will include the terms “empathy,” “clinical empathy,” and “empathy training” in all fields of the databases to establish previous literature on the empathy training program.
The protocol for this review was registered with the PROSPERO International Prospective Register of Systematic Reviews. (CRD42023400997).
Eligibility of studies
Inclusion criteria: The proposed study will include articles that detail original empirical studies and systematic reviews published only in English between 2012-2022. Studies will focus on empathy skills among health professionals and the effect of empathy training on clinical empathy skills.
Exclusion criteria: Studies with only abstracts, short reviews, guidelines, theoretical or opinion articles, and studies under low-quality criteria will be excluded from the review.
Quality appraisal
The John Hopkins EBP model will be used to assess the quality of included studies. The quality of included studies will be checked using ‘high,’ ‘medium,’ and ‘low’ descriptors. The studies that met all five criteria for quantitative and qualitative studies were termed high, while those that met three or four criteria were deemed medium. Finally, studies that met one or two criteria were classified as low. The review will focus on studies that include theoretical backgrounds to justify the contents of the interventions
Plan for data extraction
Preferred Reporting Items for Systematic Reviews and MetaAnalyses (PRISMA) will be followed to screen the studies from 2012-2022 from the selected databases. Studies, including qualitative, quantitative, and systematic reviews, will be chosen for collecting data regarding clinical empathy skills among health professionals. Study participants will be in the age group of 18 years or above.
Plan for data synthesis
The results will be narratively summarised rather than subjected to a meta-analysis because of the vast range of included study designs and results. The issues surrounding the definition of clinical empathy, clinical empathy skills among healthcare professionals, clinical empathy skills among health professional students, factors impacting clinical empathy skills, and strategies to improve clinical empathy skills will be examined methodically. Studies on empathy training to enhance clinical empathy skills among health professionals will also be a focus. The evaluation will also include research that links empathy to improvements in patient satisfaction and the standard of patient care.
Data presentation
Additionally, the study will tabulate various study features, search tactics, a process flow diagram, and forest plots of studies that will be included in the final evaluation. The information will be consistent with the goals of this systematic review. The tabulated facts and figures will accompany a narrative summary that will suggest additional research about the methodology for conducting evidence synthesis of barrier and enabler studies.
Ethical clearance: Ethical approval is not required since the study comes under systematic review, and no clinical trial registration is required as human participants are not involved
References
- Irving P, Dickson D. Empathy: towards a conceptual framework for health professionals. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2004; 17(4–5): 212–220
- Lussier MT, Richard C. Communication tips. Feeling understood: expression of empathy during medical consultations. Can Fam Physician. 2007; 53(4): 640–641.
- Hajibabaee, Fatemeh & Farahani, Mansoureh & Ameri, Zahra & Salehi, Tahmine & Hosseini, Agha. The relationship between empathy and emotional intelligence among Iranian nursing students. International Journal of Medical Education. 2018; 9: 239-243. 10.5116/ijme. 5b83.e2a5.
- Hojat M. Empathy and patient outcomes. In: Empathy in Health Professions Education and Patient Care. Springer. 2016; 189-201. doi: 10.1007/978-3-319-27625-0_11
- Gholamzadeh S, Khastavaneh M, Khademian Z, Ghadakpour S. The effects of empathy skills training on nursing students’ empathy and attitudes toward elderly people. BMC Med Educ. 2018; 18: 196. doi: 10.1186/s12909-018-1297-9
- Menezes P, Guraya SY, Guraya SS. A Systematic Review of Educational Interventions and Their Impact on Empathy and Compassion of Undergraduate Medical Students. Front. Med. 2021; 8: 758377. doi: 10.3389/fmed.2021.75837
- Weng HY, Fox AS, Shackman AJ, Stodola DE, Caldwell JZ, Olson MC, et al. Compassion training alters altruism and neural responses to suffering. Psychol Sci. 2013; 24: 1171-80. doi: 10.1177/0956797612469537
- Ilknur Kahriman, Nesrin Nural, Umit Arslan, Iran. Red Crescent Med J. 2016; 18(6): e24847. doi: 10.5812/ircmj.24847, PMCID: PMC5002343, PMID: 27621922
- Ding X, Wang L, Sun J, Li DY, Zheng BY, He SW, et al. Effectiveness of empathy clinical education for children’s nursing students: A quasi-experimental study. Nurse Educ Today. 2020; 85: 104260. doi: 10.1016/j.nedt.2019.104260. Epub 2019 Nov 6. PMID: 31778862.
- Frans Derksen, Jozien Bensing and Antoine Lagro-Janssen. British Journal of General Practice. 2013; 63 (606): e76-e84. DOI: https://doi.org/10.3399/bjgp13X660814
- Moudatsou M, Stavropoulou A, Philalithis A, Koukouli S. The Role of Empathy in Health and Social Care Professionals. Healthcare (Basel). 2020; 8(1): 26. doi: 10.3390/healthcare8010026. PMID: 32019104; PMCID: PMC7151200.
- Poorchangizi B, Borhani F, Abbaszadeh A. et al. The importance of professional values from nursing students’ perspective. BMC Nurs, 2019; 18: 26. https://doi.org/10.1186/s12912-019-0351-1
- Maria M, Areti S, Sofia K. Healthcare (Basel). 2020; 8(1): 26. doi: 10.3390/healthcare8010026, PMCID: PMC7151200, PMID: 32019104.