SciBase Journals
SciBase Epidemiology and Public Health
ISSN 2996-4555
- Article Type: Research Article
- Volume 2, Issue 1
- Received: Nov 22, 2023
- Accepted: Feb 14, 2024
- Published Online: Feb 21, 2024
Knowledge, attitudes and practices of health care workers regarding the prevention of nosocomial infections in the ICU
Bengono Bengono RS1,2*; Jemea B1,3; Amengle AL1,4; Ndom Ntock F1,5; Iroume C1,3; Lemoula G4; Kona Ngondo S1,6; Ze Minkande J1,4
1Department of Surgery and Specialties, Faculty of Medicine and Biomedical Sciences, Yaoundé, Cameroon.
2Intensive Care Unit, Reference Hospital of Sangmelima, Sangmelima, Cameroon.
3Intensive Care Unit, Yaoundé Teaching University Hospital, Yaoundé, Cameroon.
4Intensive Care Unit, Yaoundé Gynaeco-Obstetric and Pediatric Hospital, Yaoundé, Cameroon.
5Intensive Care Unit, Douala General Hospital, Douala, Cameroon.
6Intensive Care Unit, Yaoundé N°1 Military Hospital, Yaoundé, Cameroon.
*Corresponding Author: Bengono Bengono RS
Intensive Care Unit, Reference Hospital of Sangmelima, Cameroon.
Email: rodbeng@yahoo.fr
Abstract
Background: The aim of this study was to evaluate the knowledge, attitudes and practices of health care personnel regarding the prevention of nosocomial infections in the ICU.
Methods: This was a cross-sectional, descriptive, study that took place in the intensive care units of two university hospitals of Yaoundé. Our study was conducted in two phases: the first phase consisted of the administration of an anonymous, self-administered questionnaire to the health care personnel who agreed to participate in the study, and the second phase permitted us to evaluate the personnel’s’ practices using the WHO model observation form. Data analysis was done using CS-Pro version 7.5, Microsoft® Office Excel 2013 and S.P.S.S. 21.0.
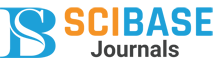
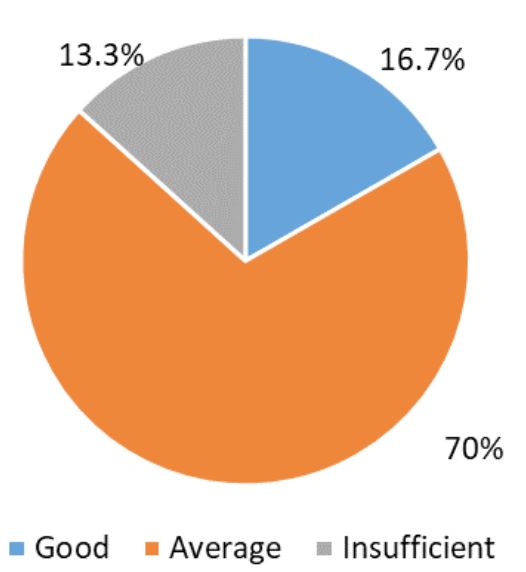
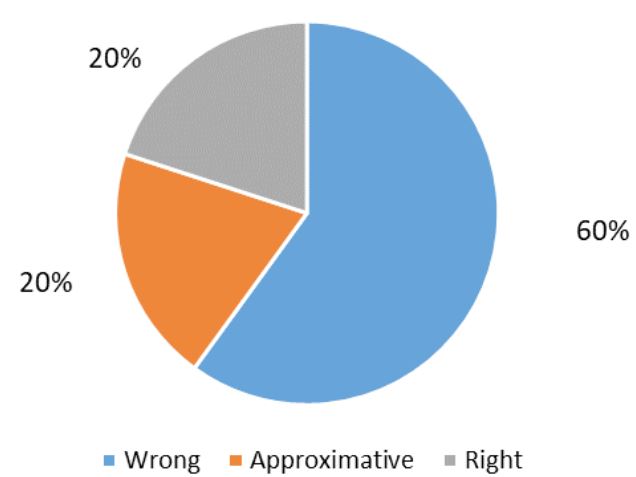
Results: Our sample consisted of 60 practitioners. The sex-ratio was 0.54. The mean age was 38.35 ± 8.86 years. Most of the staff had been in the ICU for less than 5 years and only 35% of the staff had received at least one continuing education course on infection control measures. Good knowledge was found in 70% of the staff assessed, 60% had incorrect attitudes, and 63% had inadequate practices. The rate of compliance with good hygiene practices was 55.2%.
Conclusion: Knowledge were mean, attitudes were wrong and practices were inadequate regarding the management of nosocomial infections in the ICU.
Keywords: Knowledge; Attitudes; Practices; Health care worker; Nosocomial infection; ICU.
Citation: Bengono Bengono RS, Jemea B, Amengle AL, Ndom Ntock F, Iroume C, et al. Knowledge, attitudes and practices of health care workers regarding the prevention of nosocomial infections in the ICU. SciBase Epidemiol Public Health. 2024; 2(1): 1018.
Introduction
Nosocomial infection, also known as a hospital acquired infection, is an infection if it becomes positive 48 hours or more after admission to the hospital or within 30 days of discharge. Nosocomial infection in healthcare facilities is a major public health problem in most developing countries [1-3]. The high incidence and morbidity in the ICU is related to the density of care, exposure to various invasive devices and the severity of the patients’ pathologies. The universal incidence is about 5-8% of admitted patients, of which one third are preventable [2]. Nosocomial infections are an important public health problem in many developing countries, particularly in the intensive care unit (ICU) [4]. In Africa, healthcare-associated infections were estimated in 2010 by the WHO to affect between 5 and 15% of hospitalized patients. These infections could affect between 9% and 37% of patients admitted to ICU [5].
In Cameroon, a study conducted in the ICU of Laquintinie Hospital in Douala in 2012 by Njall et al shows a prevalence of 12% [6]. According to a study conducted by Thiago et al in Brazil in 2007, the intensive care unit is the unit with the highest prevalence of nosocomial infections with a percentage of 29% [7]. A similar study by Latifa et al in Tunisia in 2014 showed an incidence of 30.8% of nosocomial infections [8]. Mortality due to nosocomial infections can reach 34.2% with an additional 14 days of hospitalization according to a study conducted by Rosenthal et al in [3] ICU in Argentina in 2003 [4].
A high frequency of nosocomial infections is always an indicator of poor quality of health care facilities [9]. The determinants of healthcare-associated infections in emerging countries are lack of infrastructure, insufficient equipment, inadequate hygiene conditions, non-application of protocols, inappropriate use of antibiotics, lack of respect for hygiene, and insufficient knowledge of healthcare professionals, which may be due to lack of initial training [10]. Infections contracted on the wards are major risk factors that increase the morbidity of hospitalized patients. In fact, they place a heavy burden on patients and community health, and there is evidence that they can prolong the length of stay [11]. Healthcare-associated infections are a common consequence of unsafe health care practices and are a major issue for patient safety. Health care workers play a key role in patient safety and the quality of care, with factors such as poor compliance with hygiene standards and poor knowledge of infection risks having a major impact. However, the role of health care workers in patient safety has been overlooked in the literature [12]. The aim of this study was to assess the knowledge, attitudes and practices of health care workers (HCW) regarding the prevention of NI in the ICU.
Methods
This was a cross-sectional, descriptive knowledge, attitude and practice (KAP) study. The study took place in the ICU of the Yaoundé Gynaeco-Obstetric and Paediatric Hospital (YGOPH) and the Yaoundé University Hospital (YUH). Data collection took place from 22 February to 22 May 2021. The study included all HCWs of both sexes working in the intensive care units of the selected hospitals, all health care workers present during the study period and all personnel who gave their consent to participate in the study. Not included in the study were any health care workers who were absent during the study period and any personnel who did not give their consent to participate. We used exhaustive consecutive sampling for healthcare staff. The minimum sample size was estimated using the Cochrane proportion estimation formula. The prevalence of NI was 4% according to Mufuka et al. in Congo [13]. The minimum sample size calculated was 59 HCWs.
After approval from the Institutional Ethics and Research Committee of the Faculty of Medicine and Biomedical Sciences (FMBS) of the University of Yaoundé I, the recruitment began. The study was divided into two parts. The first part consisted of an interview in which a pre-designed questionnaire was administered. It consisted of 59 questions organized under [4] headings. It made it possible to identify the socio-professional characteristics of health workers, their knowledge, attitudes and practices regarding the management of NI. The evaluation of knowledge, attitudes and practices was done by adding up the number of points obtained by each answer in the questionnaire. Each correct answer was worth two points, approximate answers one point and wrong answers zero points. Overall knowledge was characterized as poor (< 50% correct answers), insufficient (50-65%), average (65-85%) and good (>85%). Regarding global attitudes, they were characterized as bad (< 50% correct), wrong (50-65%), approximate (65-85%) or right (>85%). For the overall practices, they were characterized as bad (< 50% correct answers), inadequate (50-80%) and adequate (>80%). The second part of the study assessed the practices of the health personnel. It was carried out using an observation grid with the following items: professional dress, hygiene, wearing of gloves, hand rubbing with a hydro-alcoholic solution and hand washing. Each staff member was assessed over a period of 30 minutes. At the end of this assessment, practices were judged to be good (percentage of calculated score ≥ 85%), average (60 - 85%) and poor (percentage of score < 60%). Data were entered and coded in CSPro (Census Survey Processing) version [7.5]; then extracted to S.P.S.S. (Statistical Package for Social Sciences) version [21.0] for statistical analysis. Graphs were constructed using Microsoft® Office Excel 2013 and S.P.S.S. 21.0. Positional parameters such as mean and median, and dispersion parameters such as standard deviation and interquartile ranges, were used to describe continuous variables. Categorical variables were described in terms of frequency and percentage. Informed consent was obtained from each participant before inclusion in the study. The information collected was kept under strict medical confidentiality and used only for scientific purposes.
Results
The sample size consisted of 60 health care workers. The mean age was (38.35 - 8.86) years with extremes ranging from (25) to (58) years. The age range (25-34) was predominant (41.7%). Female HCWs, representing 65%, the sex-ratio was (0.54). Married HCWs represented 63.3% and nurses represented 36.7% of the sample. HCWs with less than one year of service were the most represented group (31.7%).
Knowledge: Regarding the definition of an NI, it was adequate in 96.7% of cases. The correct definition was found in 83.3% of cases. Patients were considered to be the group most susceptible to infection. Nurses were the group most likely to transmit a NI to patients at 61.1%. The pathogen responsible for the infection was bacteria in 93.3% of cases. The majority of the sample (90%) thought that NIs were transmitted by medical equipment. When asked if they knew the methods of prevention of infection, 56/60 or 93.3% answered yes. Correct answers regarding the signs and symptoms of infection were found in 58.3% of the cases. The majority of HCWs (65%) had not received any refresher training since their training. Training was between (6-12) months old for 9 HCWs (42.9%). Knowledge was average for 70% of HCWs.
Attitudes: He majority of HCWs (93.3%) felt that every patient should be considered a carrier of a pathogen that can be transmitted through blood or other biological secretions. Hand care materials were always available in 36.7% of cases. Hand hygiene materials caused irritation and dryness according to 85% of the HCWs. The population found the application of disinfection guidelines/procedures very useful in 61.7% of cases. Half of the population often forgot to wash their hands. Recyclable material was sterilized according to 43% of the HCWs. Comfort in performing care was not optimal for 28.3% of the sample. Attitudes were wrong for 60% of the participants.
Practices: The majority of HCWs health (80%) respected asepsis before opening a wound. Non- compliance with preventive measures was found among 81.7% of HCWs. Only 35% of the participants cleaned their gowns after a shift in hospital. Jewellery were removed by 53.3% of the HCWs when washing their hands. The health care workers washed their hands between two patients in 80% of cases. Needles could be recapped after use by 56% of participants. The difficulties described by 90% of the HCWs in carrying out care and medical acts were the lack of hospital consumables and the inadequacy between the quantity of HCWs and the workload. Physical measures and injection of antipyretics were performed in case of fever by 65% of the staff. Inadequate practices were found in 63% of the sample.
Compliance with hygiene practices: Hygiene practices during care were observed in 35 HCWs. Observation of the hygiene practices of the HCWs showed 97.1% wearing a gown (high level of compliance), 68.6% wearing gloves during high-risk procedures (medium level), regarding hand rubbing only 22.9% did it and only 1 mastered the technique, 51.4% (18/35) who washed their hands, of which 1/9 mastered the hand washing technique (low level) The score obtained by the HCWs for the criteria concerned was 55.2%. Health care workers had a low level of compliance with hygiene and infection control methods
Table 1: Socio-demographic data.
| Variables | Number (n) | Percentage (%) |
|---|---|---|
| Hospital | ||
| YCH | 28 | 46.7 |
| YGOPH | 32 | 53.3 |
| Age (years) | ||
| 25 - 34 | 25 | 41.7 |
| 35 - 44 | 19 | 31.7 |
| 45 and above | 16 | 26.7 |
| Gender | ||
| Male | 21 | 35 |
| Female | 39 | 65 |
| Marital status | ||
| Single | 22 | 36.7 |
| Married | 38 | 63.3 |
| Professionnal category | ||
| Nursing Assistant | 2 | 3.3 |
| Nurse | 22 | 36.7 |
| Anesthetic nurse | 14 | 23.3 |
| General practitioner | 1 | 1.7 |
| Anesthesiologist | 4 | 6.7 |
| Resident | 17 | 28.3 |
| Years of service in ICU | ||
| < 1 | 19 | 31.7 |
| 1 – 5 | 12 | 20 |
| 6 – 10 | 15 | 25 |
| 11 and above | 14 | 23.3 |
Table 2: knowledge regarding prevention of NI.
| Knowledge | Number | Percentage (%) |
|---|---|---|
| NI’s meaning | ||
|
A NI is an infection that
the patient contracts in hospital that was not present on admission and whose first signs and symptoms appear at least 48 hours after admission |
50 | 83.3 |
| Incomplete meaning | 10 | 16.7 |
| Most NI-sensitive group | ||
| Patient | 48 | 80 |
| Nurse | 8 | 13.3 |
| Surface technician | 3 | 5 |
| Doctor | 1 | 1.7 |
| Group most likely to transmit NI | ||
| Nurses | 37 | 61.7 |
| Visitors | 8 | 13.3 |
| Doctors | 7 | 11.7 |
| Surface technician | 4 | 6.7 |
| Nursing Assistant | 2 | 3.3 |
| Laboratory technician | 2 | 3.3 |
| Pathogens causing NI | ||
| Bacteria | 56 | 93.3 |
| Virus | 2 | 3.3 |
| Fungi | 2 | 3.3 |
| Knowledge concerning prevention’s method of NI | ||
| Yes | 56 | 93.3 |
| No | 4 | 6.7 |
| Prevention’s methods of NI cited by health care workers (N=56) | ||
| Hand washing | ||
| Yes | 56 | 100 |
| No | / | / |
| Personal protective equipment (apron, mask cover, shoe cover, gloves) | ||
| Yes | 53 | 94.6 |
| No | 3 | 5.4 |
| Sterilization | ||
| Yes | 49 | 87.5 |
| No | 7 | 12.5 |
| Health care workers who have received NI control training | ||
| Yes | 21 | 35 |
| No | 39 | 65 |
| Date of last training course (month) | ||
| 1 – 5 | 5 | 23.8 |
| 6 – 11 | 9 | 42.9 |
| 12 – 23 | 3 | 14.3 |
| 24 and above | 4 | 19 |
Table 3: knowledge regarding prevention of NI.
| At+A1:C18titudes | Number (n) | Percentage (%) |
|---|---|---|
| Perceived risk of contracting a disease during care | ||
| High risk | 28 | 46.7 |
| Medium risk | 31 | 51.6 |
| No risk | 1 | 1.7 |
|
Every patient should be
considered a carrier of a
pathogen transmissible through blood or other biological secretions |
||
| Yes | 54 | 90 |
| No | 6 | 10 |
| Hand care materials were always available | ||
| Yes | 22 | 36.7 |
| No | 38 | 63.3 |
| The application of the guidelines was very useful for the prevention of NI | ||
| Yes | 37 | 61.7 |
| No | 23 | 38.3 |
| Hand hygiene was forgotten or not performed | ||
| Yes | 30 | 50 |
| No | 30 | 50 |
| Is comfortable with infection control practices in the health care facility | ||
| Yes | 25 | 41.7 |
| No | 35 | 58.3 |
| Sterilization of recyclable care materials is always done | ||
| Yes | 26 | 43.3 |
| No | 34 | 56.7 |
|
Adherence to preventive
measures in case of
increased workload or emergency |
||
| Yes | 49 | 81.7 |
| No | 11 | 18.3 |
| Systematic cleaning of gowns after shift | ||
| Yes | 18 | 30 |
| No | 42 | 70 |
Table 4: Practices concerning prevention of NI.
| Practices | Number (n) | Percentage (%) |
|---|---|---|
|
Did you follow the
recommended guidelines for
the use of alcohol-based solutions or other antiseptics before opening the vascular access? |
||
| Yes | 48 | 80 |
| No | 12 | 20 |
| Do you cover the nose and mouth when sneezing? | ||
| Yes | 57 | 95 |
| No | 3 | 5 |
| Do you use a mask before approaching a patient? | ||
| Yes | 58 | 96.7 |
| No | 2 | 3.3 |
| Compliance with preventive measures in case of increase workload | ||
| Yes | 11 | 18.3 |
| No | 49 | 81.7 |
| Cleaning the gown after the shift | ||
| Yes | 21 | 35 |
| No | 39 | 65 |
| Wearing jewellery during hand washing | ||
| Yes | 28 | 46.7 |
| No | 32 | 53.3 |
| Do you wash your hands between patients? | ||
| Yes | 48 | 80 |
| No | 12 | 20 |
| Do you wash your hands before contact with the patient? | ||
| Yes | 38 | 63.3 |
| No | 22 | 36.7 |
Table 5: Compliance level of hygiene practices of 35 health care workers.
| Indicators | Criteria | Level of scores | Overall Level (%) | Compliance level | |
|---|---|---|---|---|---|
| N=35 | % | ||||
| Professional dress | Wearing the gown | 34 | 97.1 | 84.9 | Good |
| Clean gown | 28 | 82.3 | |||
| Short sleeve gown | 26 | 74.3 | 8.6 | Average | |
| Wearing gloves | During high-risk care | 24 | 68.6 | ||
| Hand rubbing | Practice hand rubbing | 8 | 22.9 | 20.6 | Low |
| Mastering the technique | 1 | 2.9 | |||
| Hand washing | Practice hand washing | 18 | 51.4 | 46.8 | Low |
| Mastering the technique | 2 | 5.7 | |||
| 55.2 | Low | ||||
Discussion
The main limitation of our study was the sample size. This was secondary to the low number of health care workers at the ICU in our context. The other limitation was the type of study. It was a multicenter study. This allowed us to have a usable sample. However, this type of study can pose a selection bias with the divergence of practices in two different hospitals.
The mean age was 38.35 ± 8.86 years and the sex-ratio was 0.54. This was similar to the sample found by Hien et al in 2013 in Burkina Faso. They found a mean age of 36.6 ± 5.72 and 64.6% female HCWs [12]. Majority (70.7%%) of the participants belonged to 18 to 25 years age group [14]. Most of the participants were female 231 (96.3%) in the sample of Jahangir study [15]. The most represented professional category was nurses (36.7%). These results were similar to others series [1-3,12,14- 15]. The majority of HCWs (31.7%) had less than one year of service in the ICU. This was different from the data of Derraji in 2013 in Morocco who found a proportion of 60% of the staff having worked for less than five years in the ICU [16].
Regarding knowledge, the definition of nosocomial infection was correct in 83.3% of cases. This was different from the results of Mufuka et al in the Democratic Republic of Congo. They found that 4% of staff gave a correct definition of nosocomial infection [13]. The difference between the two studies could be explained by the heterogeneous study population, consisting of residents, doctors and nurses in our sample. Hien et al found that 30.04% of the health care workers knew the definition of healthcare-associated infections [12]. The nurse group was the most likely to transmit an infection to patients (65%). These results were consistent with those obtained by Kaushik et al in 2018 in India, where they found the majority of the nurses group (34.6%) [17]. Only 44.4% of the HCWs reported that the hands (in the event of poor hand hygiene compliance) were the main mode of transmission of germs between patients in a care facility [12]. Bacteria were the pathogens most responsible for NI according to 93.3% of the participants. This was similar to the findings of Kaushik et al in India, who found in 2018 that 56.6% of the staff had thought of bacteria [17]. The means of transmission of NCIs was represented by medical equipment according to 90% of the participants. This was also found by 85% of participants in the study by Kaushik et al [17]. Regarding the prevention of NI, 93.3% of the staff knew the methods of prevention, 88.3% noted that hand treatment was the best method of prevention and 81.7% had well defined sterilization. These results were similar to those of many African series. Okowii et al in Uganda [18] and Kaushik et al [17] found that 84.3% of the participants knew the prevention methods, and 88.6% had correctly defined sterilization. The overall level of knowledge was moderate (70%). Jahangir et al. revealed that nurses have enough knowledge about spread of nosocomial infection [15]. The results of the study of Atika et al. showed that HCWs had adequate knowledge regarding hospital acquired infection [19]. A study conducted in Ethiopia among 150 health care workers working in a hospital, found that 84% participants had good knowledge of infection prevention [20]. Another study conducted in Nigeria regarding infection control knowledge and practices among HCWs, 200 (doctors and nurses) participants were included in the study. 87% respondents identified that hand hygiene was the most effective barrier to control NI. They had good knowledge [21]. Nag et al. showed that, 87.4% healthcare personnel have some knowledge about Hospital Acquired Infection [14]. Most of the nurses (87%) had a fair level of knowledge, while only 4% of them had a good level of knowledge of preventive measures of nosocomial infections [22].
Regarding attitudes, the risk of transmitting an infectious disease to a patient was known by 18.3% of the participants. This was different from the data found by Okwii et al. The practitioners evaluated recognized the risk of transmitting an infectious disease to a patient in 36.4% of cases [18]. Each patient should be treated as if he or she was a carrier of a pathogen transmissible through biological secretions according to 93.3% of the participants. Okwii et al, found similar data [18]. Half of the population studied often forgot to perform hand hygiene. Okwii et al found 17% of cases of forgetfulness [18]. Materials (gel, soap, water, gloves) for hand care were available in 36.7% of cases. This was similar to the data of Kaushik et al, who found availability in 41% of cases [17]. This could explain the non- compliance of the staff in observing hygiene measures. The overall level of attitudes was wrong in 60% of cases. This could be explained by the beliefs of the HCWs and the difficulties described.
Regarding practices, the majority of HCWs (80%) respected asepsis before inserting a venous line. They covered their nose and mouth during sneezing (78%). A mask was used when approaching the patient (96.7%). Kaushik et al, reported similar results. Recommendations for prevention of NI were not followed by 81.7% of participants in case of increased workload or in case of emergency [17]. Maria et al in 2017 in Pakistan also found 83.3% non-compliance in emergency situations [15]. The lack of HCWs in the two ICU studied and the workload could explain these harmful practices. Gowns were cleaned after a shift in 35% of cases. Hand washing before patient contact was performed by 63.3% of the participants, 91.7% after contact and 80% between the two patients. Mufuka et al. found that 29.3% of staff washed their hands before contact with the patient, 49.5% after contact [13]. Nag et al, showed that most of the study participants washed their hands after handling the patients (90.2%) [14]. The majority of HCWs (90%) reported the following difficulties in adequately carrying out the prevention of infection during care: lack of consumables and high workload. The overall practices were inadequate for 63.34% of HCWs. Hien et al found harmful practices in a similar study [12]. In Ethiopia, Desta et al, found that HCWs had inadequate practices regarding infection prevention [20]. Their practices were not good regarding standard isolation precautions and hand hygiene [21].
Regarding compliance with practices, the score obtained for all relevant criteria was 55.2%. Health professionals had a low level of compliance with hygiene and infection control methods. Our results were similar to data from other African series. Mufuka et al in the Democratic Republic of Congo [13] and Hien et al, in Burkina Faso [12], also found low levels of compliance with hygiene protocols. It was 38.25% and 36.85% respectively. This could be explained by the wrong level of attitudes, the lack of equipment and consumables for care and the lack of training. In addition, there was the absence of functional hand washing devices in the wards, the absence or non-application of protocols and procedures for hygiene techniques, and the inadequacy of supervision and continuous training. A total of 236 participants were included in the study of Bayleyegn B et al. Only 36% of the study participants had good practices towards health acquired infections prevention. Additionally, hospitals should provide infection prevention facilities and supplies, continuous water supply, hand washing sinks and all necessary personal protective equipment to improve infection prevention practices of healthcare workers [23]. There are many reasons such as increasing inpatient activity of illness, inadequate nurse patient staffing ratios, unavailability of system resources and other demands have challenged heath care providers. Preventions of nosocomial infection is the responsibility of all individuals and health care providers. For the promotion of good health care appropriate isolation, sterilization, other practices and adequate staff training should be necessary [19]. Healthcare workers play a significant role in spreading the infection and they are regarded as key members of managing and controlling the hospital infections; thus, healthcare workers must have correct, up-to date and appropriate scientific information regarding varieties of hospital infections, their effects on afflicting patients, and increased hospital costs, recognition of people at risk and also the criteria to prevent and control. On the other hand, HCW knowledge and practices regarding sanitary conditions play a vital role to guarantee the individual and ultimately social health, increased level of HCW knowledge positively affects their performance [24].
Conclusion
Nosocomial infection is one of the major global burden on health. Health care workers play major role in prevention of infection from themselves and their patients. HCWs had average knowledge, erroneous attitudes and inadequate practices regarding the prevention of nosocomial infections in the ICU. The promotion of patient safety and quality of care requires a focus on training and behavior change among HCW. The gaps in knowledge and practices regarding NI control measures indicate the need to establish a related health care policy regarding NIs and implement a regular training program to upgrade and refresh the HCWs’ knowledge, attitudes and practices regarding NI control measures. Importance of prevention of NI should be emphasized among HCWs by intensive IEC activities.
Conflicts of interest: The authors declare no conflicts of interest.
Authors’ contributions: All authors contributed to the design and conduct of this study. All authors have read and approved the final version of the manuscript.
References
- Etiz P, Yüzbaşıoğlu-Arıyürek S. Assessment of knowledge about nosocomial infection among Cukurova University Vocational School of Health Services Students. Turk Hij Den Biyol Derg. 2020; 77(1): 69-78.
- Dutta V, Bora I, Khyriem A, Phukan A, Durairaj E. Study of Nosocomial Infections among the Patients Admitted in the Intensive Care Units of a Tertiary Care Centre in North East India. International Journal of Scientific Research. 2017; 6: 55-60.
- Alrubaiee et al. Knowledge and practices of nurses regarding nosocomial infection control measures in private hospitals in Sana’a City, Yemen. Safety in Health. 2017; 3: 16.
- Rosenthal VD, Guzman S, Orellano PW. Infections nosocomiales dans les unités de soins intensifs médico- chirurgicaux en Argentine mortalité et durée de séjour. Am j infect control. 2003; 31: 291-5.
- OMS. Résumé des Recommandations de l’OMS pour l’Hygiène des Mains au cours des Soins. Premier Défi Mondial pour la Sécurité des Patients. Un Soin propre est un Soin plus sûr.2010. [consulté le 22 janvier. 2021. disponible: https://apps.who.int/iris/bitstream/handle/10665/70469/WHO_IERSP_2009.07_f e.pdf? sequence=1.
- Njall C, Adiogo D, Bita A, Ateba N, Sume G, Kollo B, et al. Écologie bactérienne de l’infection nosocomiale au service de réanimation de l’hôpital Laquintinie de Douala, Cameroun. Pan Afr Med J. 2013; 14. Disponible à l’adresse: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3683522/
- Lisboa T, Faria M, Hoher JA, Borges LAA, Gómez J, Schifelbain L, et al [The prevalence of nosocomial infection in Intensive Care Units in the State of Rio Grande do Sul]. Rev Bras Ter Intensiva. 2007; 19: 414-20.
- Merzougui L, Bahroumi T, Guizani T. Les infections nosocomiales en milieu de réanimation : incidence annuelle et aspects cliniques au service de réanimation polyvalente, Kairouan, Tunisie, 2014. The Pan African Medical Journal. 2018; 30: 9.
- Assiri AM, Choudhry AJ, Alsaleh SS, Alanazi KH, Alsaleh SS. Evaluation of Infection Prevention and Control Programmes (IPC), and Assessment Tools for IPC-Programmes at MOH-Health Facilities in Saudi Arabia. Open Journal of Nursing. 2014; 4(7): 720-6.
- Revelas A. Healthcare - associated infections: Un problème de santé publique. Niger Med J. 2012; 53(2): 59- 64.
- Memish ZA. Infection control in Saudi Arabia: meeting the challenge. Am J Infect Control. 2002; 30(1): 57-65.
- Hien H, Drabo M, Ouédraogo L, Konfé S, Sanou D, Zéba S et al. Knowledge and practices of health care workers in the area of healthcare-associated infection risks. A case study in a district hospital in Burkina Faso. Santé Publique. 2013; 25 (2): 219- 226.
- Mufuka k. Evaluation des connaissances, attitudes et pratiques du personnel soignant sur le risque nosocomial à la clinique ngaliema en République Démocratique du Congo. European Journal of Public Health Studies. 2020; 2(2): 10-23.
- Nag K, Datta A, Karmakar N, Chakraborty T. Knowledge, attitude and practice about hospital acquired infection among health care personnel in a tertiary care hospital of Tripura. Int J Res Med Sci. 2018; 6(10): 3303-3308.
- Jahangir M, Ali M, Riaz MS. Knowledge and Practices of Nurses Regarding Spread of Nosocomial Infection Ingovernment Hospitals, Lahore. J Liaquat Uni Med Health Sci. 2017; 16(03): 149-53. doi: 10.22442/jlumhs.171630524.
- Derraji S , Mahila M , Baite A , Cherrah Y. et al. Hand hygiene compliance. Maroc médical. 2013; 35(4): 286-290.
- Kaushik N, Anjan D, Nabarun K, Tamal C. Knowledge, attitude and practice about hospital acquired infection among health care personnel in a tertiary care hospital of Tripura, India. Int J Res Med Sci. 2018; 6(10).
- Okwii M. Knowledge, Attitude and Practices of Nurses On Prevention And Control Of Hospital Acquired Infections In Soroti Regional Referral Hospital. International Health Sciences University; Soroti. 2017.
- Atika Akram, Sana Majeed, Habib-Ur-Rehman. Assessment of Knowledge Regarding Hospital Acquired Infections (Nosocomial Infection) Among Health Care Workers in a Tertiary Care Hospital of Wah Cantt. Saudi J Nurs Health Care. Feb. 2020; 3(2): 83-87.
- Desta M, Ayenew T, Sitotaw N, Tegegne N, Dires M, & Getie M. Knowledge, practice and associated factors of infection prevention among healthcare workers in Debre Markos referral hospital, Northwest Ethiopia. BMC health services research. 2018; 18(1): 465.
- Iliyasu G, Dayyab FM, Habib ZG, Tiamiyu AB, Abubakar S, Mijinyawa MS, & Habib AG. Knowledge and practices of infection control among healthcare workers in a Tertiary Referral Center in North-Western Nigeria. Annals of African medicine. 2016; 15(1): 34.
- Alrubaiee et al. Knowledge and practices of nurses regarding nosocomial infection control measures in private hospitals in Sana’a City, Yemen. Safety in Health. 2017; 3: 16.
- Bayleyegn B, Mehari A, Damtie D, Negash M. Knowledge, Attitude and Practice on Hospital-Acquired Infection Prevention and Associated Factors Among Healthcare Workers at University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. Infection and Drug Resistance. 2021; 14: 259-266.
- Kalantarzadeh M, Mohammadnejad E, Ehsani SR; Tamizi Z. Knowledge and practice of nurses about the control and prevention of nosocomial infections in emergency departments. Arch Clin Infect Dis. 2014; 9(4): 1827.