SciBase Journals
SciBase Neurology
ISSN 2691-7785
- Article Type: Mini Review
- Volume 1, Issue 1
- Received: Jul 21, 2023
- Accepted: Sep 01, 2023
- Published Online: Sep 08, 2023
Nutritional Assessment in Stroke Patients
Stefano Mancin RN1,2,3*; Marco Sguanci4
1Department of Biomedicine and Prevention, University of Rome “Tor Vergata”, Rome, Italy.
2IRCCS Humanitas Research Hospital, Rozzano, Milano, Italy.
3Department of Biomedical Sciences, Humanitas University, Milan, Italy.
4Department of Medicine and Surgery, Research Unit of Nursing Science, Università Campus Bio-Medico di Roma, Roma, Italy.
*Corresponding Author: Stefano Mancin RN
IRCCS Humanitas Research Hospital via Manzoni, 56 20089 Rozzano, Milano, Italy.
Tel: +44-0117-965 6261;
Email: stefano.mancin@humanitas.it
Abstract
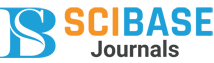
Stroke is a common acute neurological disorder that leads to significant morbidity and mortality worldwide. Malnutrition is a frequent problem among stroke patients, with a prevalence of approximately 20% at the time of hospital admission. Dysphagia, the difficulty of swallowing, is a common complication after stroke and contributes to reduced nutrient intake and increased risk of malnutrition and dehydration. Nutritional assessment plays a crucial role in the management of stroke patients, ensuring adequate nutrient intake and personalised nutritional plans. International guidelines recommend screening for malnutrition within 48 hours of hospital admission, with the Malnutrition Universal Screening Tool (MUST) recognised as suitable for acute stroke patients. In the chronic phase, ongoing assessment in the community with the participation of healthcare professionals is important. Studies have shown that the Mini Nutrition Assessment (MNA) is effective in identifying malnutrition in this phase, with strong correlations with functional outcomes. Collaboration between healthcare professionals, the multidisciplinary team, and caregivers is essential in the development of personalised nutritional plans. Nutritional assessment in stroke patients should be comprehensive, spanning from the acute phase to the chronic phase, to optimise recovery and overall well-being of patients.
Keywords: Stroke; Nutritional assessment; Malnutrition; Dysphagia.
Citation: Stefano Mancin RN, Sguanci M. Nutritional Assessment in Stroke Patients. SciBase Neurol. 2023; 1(1): 1002.
Introduction
Stroke represents one of the most common acute neurological disorders and is one of the leading causes of global mortality and disability. Each year, millions of people around the world are affected by or live with this disease, which can have severe physical, cognitive, and functional consequences [1]. The risk factors for stroke are diverse and include advanced age, hypertension, heart disease, diabetes, smoking, obesity, and an unhealthy lifestyle [2]. Patients who have suffered a stroke are at high risk of malnutrition and nutritional problems caused by various factors, predominantly associated with neurological complications [3]. Malnutrition is a common problem among stroke patients, with an estimated prevalence of approximately 20% (range 6.1% and 62%) at the time of hospital admission [4]. It can result in involuntary weight loss, along with protein energy and essential micronutrient deficiencies in the body. This condition can be attributed to various factors, including dysphagia, which is a common complication following a stroke. Dysphagia is a condition characterised by difficulties in swallowing, making it difficult or even impossible for stroke patients to adequately consume food and fluids. Dysphagia can lead to reduced nutrient and fluid intake, increasing the risk of malnutrition and dehydration. Furthermore, dysphagia increases the risk of pulmonary aspiration, which can lead to serious complications such as pneumonia [3].
Therefore, the assessment of nutritional status plays a crucial role in the care and monitoring of stroke patients. Accurate identification of the patient’s nutritional needs, including any signs of malnutrition, is essential to ensure adequate nutritional intake and optimal hydration. In addition, the evaluation of dysphagia and swallowing difficulties enables the development of a personalised nutritional plan that meets the specific needs of the stroke patient [5].
Several government and international scientific societies have developed guidelines that encompass the evaluation of nutritional status in stroke patients using validated screening tools and comprehensive clinical investigations [2,6,7-9]. This evaluation should be performed throughout all phases of the disease, starting in the acute phase during hospitalisation in stroke units and continuing after hospital discharge in the chronic phase with the support of community healthcare services. It should be carried out by a multidisciplinary team of healthcare professionals, including physicians, dietitians, speech therapists and nurses, working collaboratively to ensure a comprehensive approach to the management of malnutrition and dysphagia in stroke patients.
The aim of this mini-review is to describe nutritional assessment in post-stroke patients during both the acute and chronic phases of the disease.
Nutritional assessment in patients with acute stroke
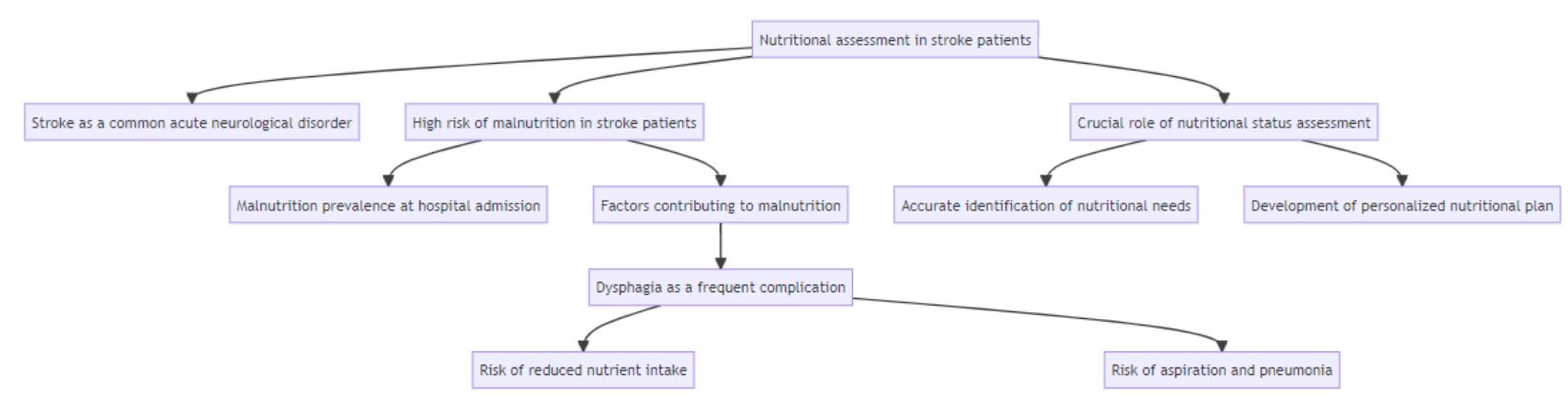
The main guidelines established by international scientific societies recommend that every patient with an acute cerebrovascular event undergoes a screening for malnutrition within 48 hours after hospital admission [2,6,7-9]. In particular, according to the guidelines of the European Society for Clinical Nutrition and Metabolism (ESPEN) [2], the Universal Malnutrition Screening Tool (MUST) is considered suitable and valid for patients in the acute phase of the disease. The Norwegian national guidelines [6] for the screening for malnutrition and acute stroke dysphagia consider the Nutrition Risk Score 2002 (NRS 2002) as an appropriate tool for use in Norwegian hospitals. The Slovenian guidelines for nutritional support in stroke [7], as well as the Canadian recommendations for good practise during hospitalization, inpatient rehabilitation, and home care after stroke [8], emphasise the importance of nutritional risk assessment without specifying a preferred tool among MUST, NRS 2002, Mini Nutrition Assessment (MNA) or Short Nutritional Assessment Questionnaire (SNAQ). Finally, the guidelines of the German Society for Clinical Nutrition (DGEM) [9] identify NRS 2002 as the most suitable screening tool for acute stroke patients, but indicate that other screening and evaluation tools, such as MUST, MNA, and Mini Nutrition Assessment (MNA-SF) may be applicable in other contexts, such as rehabilitation and home care.
Nutritional assessment in chronic stroke patients
Once a patient has experienced a stroke and is discharged from the hospital, a crucial phase in the recovery process begins. During this phase, the patient returns to his community and faces long-term convalescence, often with the need for assistance and support to improve quality of life and manage stroke-related complications [3].
To effectively address the assessment of nutritional status in this population, it is essential to involve healthcare professionals who work in the community, such as general practitioners, home nurses, dietitians, and social workers. These healthcare professionals can play a key role in the identification and evaluation for stroke patients at risk of malnutrition or nutritional problems. Through regular assessments of nutritional status, analysis of dietary intake and body weight, and identification of any signs of malnutrition, they can provide an accurate assessment of the patient's nutritional needs [10]. Furthermore, collaboration between community healthcare professionals, the multidisciplinary care team, and family/caregivers is crucial to develop personalized nutritional plans that meet the specific needs of stroke patients in the chronic phase of the disease.
In the community setting, most studies have used MNA screening tools (full or short version). The prevalence of malnutrition ranged from 22.3% to 96.7% [11-14]. The study by Kim et al. (2013) [11] found that MNA, applied to patients with chronic stroke, showed a sensitivity of 100%, a specificity of 33.3%, a positive predictive power of 81.2%, and a negative predictive power of 100%. Furthermore, compared with the MNA-SF version, MNA was found to be superior, especially when correlated with quality of life (QoL) evaluated using the WHOQOL-BREF instrument (rho=0.30, p=0.005) [12]. These findings were confirmed by a second study [13], which also evaluated the reliability of the instrument through the test-retest (ICC 0.91, [CI95% 0.85-0.94], with minimal detectable changes of 2.1% and 8.2%).
MNA also demonstrated a strong association with functional outcomes [14], such as the Motor Assessment Scale (MAS) score (r=0.4676, p=0.007), Activities of Daily Living (ADL) (r=0.24, p=0.029) and the Modified Barthel Index Score (MBI) (r=0.527, p<0.001).
Conclusion
The assessment of nutritional status in stroke patients plays a crucial role in identifying their high risk of malnutrition and addressing their specific nutritional needs. It is essential to extend the nutritional evaluation from the acute phase of the disease throughout the hospitalisation period, as well as to reevaluate it in the post-discharge phase, with the support of community healthcare professionals and local healthcare facilities. This comprehensive approach ensures that the nutritional management of stroke patients continues seamlessly, maximising their chances of recovery and improving their overall well-being.
Declarations
Funding statement: The authors received no funding for this research, neither from internal nor external bodies.
Declaration of conflict of interest: The authors declare the absence of any kind of conflict of interest.
References
- Donkor ES. Stroke in the 21st Century: A Snapshot of the Burden, Epidemiology, and Quality of Life. Stroke Res Treat. 2018; 27: 3238165.
- Burgos R, et al. ESPEN guideline clinical nutrition in neurology.” Clin Nutr 2018; 37: 354-396.
- Mancin S, Sguanci M, Reggiani F, Morenghi E, Piredda M, et al. Dysphagia screening post-stroke: systematic review. BMJ Support Palliat Care. 2023; spcare-2022-004144.
- Sabbouh T, Torbey MT. Malnutrition in Stroke Patients: Risk Factors, Assessment, and Management. Neurocritical care. 2018; 29: 374–384.
- Mancin S, Sguanci M, Cattani D, et al. Nutritional knowledge of nursing students: A systematic literature review. Nurse Educ Today. 2023; 126: 105826.
- Kampman MT, Eltoft A, Johnsen SH, et al. Full Implementation of Screening for Nutritional Risk and Dysphagia in an Acute Stroke Unit: A Clinical Audit. The Neurohospitalist, 2015; 5: 205-211.
- Klempíř, J, Šarbochová I, Růžičková, et al. “Guidelines for nutritional support in stroke.” Ceska a Slovenska Neurologie a Neurochirurgie 2020; 83: 667-673.
- Teasell, R., Salbach, N. M., Foley, N., et al. Canadian Stroke Best Practice Recommendations: Rehabilitation, Recovery, and Community Participation following Stroke. Part One: Rehabilitation and Recovery Following Stroke; 6th Edition Update 2019. International journal of stroke: Official journal of the International Stroke Society. 2020; 15: 763–788.
- Wirth R, Smoliner C, Jäger M, et al. Guideline clinical nutrition in patients with stroke. Experimental & Translational Stroke Medicine. 2013; 5: 14.
- Huppertz V, Guida S, Holdoway A, et al. Impaired Nutritional Condition After Stroke From the Hyperacute to the Chronic Phase: A Systematic Review and Meta-Analysis. Front Neurol. 2022; 12: 780080.
- Kim EJ, Yoon YH, Kim WH, et al. The clinical significance of the mini-nutritional assessment and the scored patient-generated subjective global assessment in elderly patients with stroke. Annals of Rehabilitation Medicine. 2013; 37: 66-71.
- Lee YC, Chiu EC. Nutritional status as a predictor of comprehensive activities of daily living function and quality of life in patients with stroke. Neuro Rehabilitation. 2021; 48: 337-343.
- Lin SC, Lin KH, Lee YC. Test-retest reliability of the Mini Nutritional Assessment and its relationship with quality of life in patients with stroke. PLoS One. 2019; 14.
- Weun, C. C., Hasnan, N., Latif, L. A., et al. Nutritional status of post-acute stroke patients during rehabilitation phase in hospital. Sains Malaysiana. 2019; 48: 129-135.