SciBase Journals
SciBase Obstetrics and Gynecology
ISSN 2691-7785
- Article Type: Case Report
- Volume 1, Issue 1
- Received: Aug 11, 2023
- Accepted: Sep 14, 2023
- Published Online: Sep 19, 2023
Multiple Anogenital Cancers in a 26-Year-Old Female: A Case Report
Grace Lee1; Laurie Elit2,3; Calvin Ngalla2; Florence Manjuh2; Richard Bardin2 ; Simon Manga1,2*
1Department of Obstetrics & Gynecology, The University of Alabama at Birmingham School of Medicine, 1700 6th Avenue South, Suite 10270, Birmingham, AL 35233, USA.
2Cameroon Baptist Convention Health Services, Bamenda, P.O. Box 1, Nkwen, Bamenda, Cameroon.
3Department of Obstetrics and Gynecology, McMaster University, Hamilton, ON L8V 5C2, Canada.
*Corresponding Author: Simon Manga
Email: smanga@cbchealthservices.org & smanga@uab.edu
Abstract
High-risk Human Papillomavirus (HPV) infections cause squamous intraepithelial lesions which act as precursors to invasive cancers. Due to the integration of HPV into host DNA, patients who have been diagnosed with HPV-associated invasive or preinvasive tumors may have a five-to-ten-fold increased risk of a second HPV-associated cancer, with a particularly strong association between anal and vulvovaginal cancers. This is a case report of a 26-year-old HIV-negative nulliparous female who developed independent squamous cell cancers of the vulvar, vaginal, cervix, and anus within a 2-year time frame in Cameroon. HPV specimens collected from the vagina and anus, and genotyped using the AmpFire HPV analyzer, revealed the presence of HPV Types 33, 51, and 68. Worldwide, HPV types 16 and 18 have been noted as the most virulent HPV types. Neither of these types was present in this patient with aggressive HPV-associated cancers. It is not known if the combination of these three types; 33, 51, and 68 forms a particularly virulent association in this population. This case demonstrates the importance of investigating less common high-risk HPV types and associated pathologies in this population. HPV genotypes other than 16 and 18 may play a significant role in cancer development in this population.
Keywords: Anogenital cancer; Cameroon; Female; Human Papillomavirus; Squamous Intraepithelial lesion.
Abbreviations: CBCHS: Cameroon Baptist Convention Health Services; CIN: Cervical Intraepithelial Neoplasia; DC: Digital Cervicography; HPV: Human Papillomavirus; LLETZ: Large Loop Excision of the Transformation Zone; LMIC: Low- and Middle-Income Countries; MBH: Mbingo Baptist Hospital; TZ: Transformation Zone; VAIN: Vaginal Intraepithelial Neoplasia; VIA: Visual Inspection with Acetic Acid; VILI: Visual Inspection with Lugol’s Iodine; WHP: Women’s Health Program.
Citation: Lee G, Elit L, Ngalla C, Manjuh F, Manga S, et al. Multiple Anogenital Cancers in a 26-Year-Old Female: A Case Report. SciBase Obstet Gynecol. 2023; 1(1): 1001.
Introduction
High-risk Human Papillomavirus (HPV) types cause about 5% of cancers worldwide, with cervical cancer being the leading cause of cancer-related deaths in Low- and Middle-Income Countries (LMICs) [1]. There are over 200 strains of HPV, but 14 to 15 high-risk genotypes have been identified including 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68. HPV 16 and 18 are the predominant high-risk types, causing about 50% of HPV-related neoplasia worldwide [2]. The WHO estimates that 90% of new cases and deaths from cervical cancer occurred in LMICs in 2020, particularly in sub-Saharan Africa [3]. High-risk HPV is also responsible for cancers of the anus, vagina, vulva, throat, mouth, and penis with types 16 and 18 most commonly implicated [4].
Data on HPV genotypes prevalence and their effects are lacking in LMICs. In Cameroon, studies have shown a high prevalence of high-risk HPV with reports of 21.4% to 38.5% prevalence [5]. The high burden of disease demonstrates the importance of discriminating between genotypes in order to adequately vaccinate the population at risk. One study demonstrated a predominance of genotypes 16, 18, 39, and 58, which shows high heterogeneity in the distribution of HPV types [5]. There are three approved HPV vaccines that vary in their coverage of HPV types. The bivalent HPV vaccine covers HPV 16 and 18, the quadrivalent vaccine covers 6, 11, 16, and 18, and the 9-valent vaccine covers types 6, 11, 16, 18, 31, 33, 45, 52, and 58 [6]. In Cameroon, similar to other LMICs, the quadrivalent HPV vaccine is distributed.
High-risk HPV infections cause squamous intraepithelial lesions which act as precursors to invasive cancers. These are characterized by location into Cervical Intraepithelial Lesions (CIN), Vulvar Intraepithelial Neoplasia (VIN), and Vaginal Intraepithelial Neoplasia (VAIN). Low-grade lesions are characterized as 1 (e.g., CIN1), and high-grade lesions are notated as 2 or 3. The pathophysiology of infection with HPV involves the integration of HPV DNA into host DNA and suppression of cell cycle checkpoints as well as uncontrolled cell proliferation by inactivation of host p53 and retinoblastoma protein (pRb) by E6 and E7 [7].
Due to the integration of HPV into host DNA, patients who have been diagnosed with HPV-associated invasive or preinvasive lesions may have a five-to-ten-fold increased risk of a second HPV-associated cancer, with a particularly strong association between anal and vulvovaginal cancers [8].
The Cameroon Baptist Convention Health Services (CBCHS), a large faith-based healthcare organization in Cameroon runs the largest cervical cancer prevention program in Cameroon called the Women’s Health Program (WHP). The program which relies principally on visual screening methods has been described in detail in our previous work [9]. Beginning in 2020, WHP started doing HPV screening as the primary screening test for women 30 years and older using AmpFire. The AmpFire developed by Atila Biosystems is a simple and fast HPV detection technology that uses multiplex isothermal real-time fluorescent detection. This novel HPV screening technology can detect HPV directly from raw samples, such as dry swab samples. The assay detects 15 high-risk HPV types. The time from sample to result is about an hour [10].
Case presentation
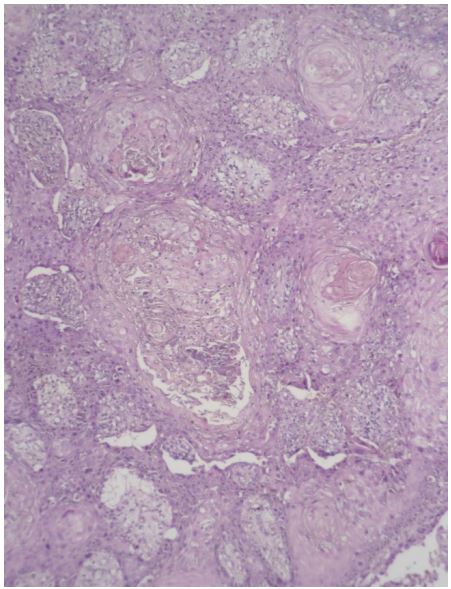
This is a case of a 26-year-old HIV-negative nulliparous female who developed independent squamous cell cancers of the vulvar, vaginal, cervix, and anus within a 2-year time frame. Her medical history was notable for asymptomatic hepatitis B infection. She initially presented at the Women’s Health Program (WHP) of the Cameroon Baptist Convention Health Services (CBCHS) in August 2019 with a two-month history of a painful vulvar lesion which had been treated unsuccessfully as vulvar condyloma by gynecologists and dermatologists at several hospitals. Some of the treatments she received included podophyllin, cauterization, Fucidin, and Betadine. On examination of the vulva, there was a tender, slightly raised, skin-colored lesion that resembled vulvar condyloma (Figure 1). Biopsies were taken with a Tischler punch biopsy forceps under local anesthesia. At the same visit, cervical cancer screening was done using Visual Inspection with Acetic acid and Lugol’s Iodine (VIA/VILI) enhanced by Digital Cervicography (DC). Findings were notable for thick and raised acetowhite epithelium covering the entirety of the Transformation Zone (TZ) of the cervix and entering into the external os beyond view, meeting the criteria for Large Loop Excision of the TZ (LLETZ).
The pathology report of the vulvar biopsy demonstrated invasive squamous cell carcinoma of the vulva. She was referred to a gynecologic oncologist at Mbingo Baptist Hospital (MBH), one of the largest hospitals of the CBCHS, and underwent a radical vulvectomy and bilateral groin node dissection in November 2019 (Figure 2). Surgical histopathology showed well-differentiated invasive squamous cancer of the vulva with margins all negative with 2 left and 3 right groin nodes negative for disease. At the time of the vulvectomy, a LLETZ was done which came out CIN3 on histopathology. The first postoperative follow-up visit at 6 months was unremarkable (Figure 3).
The patient presented again in WHP in June 2021 with a raised, painful, perianal verrucous lesion resembling the initial vulvar lesion and having a radius of approximately 3 cm from the anus (Figure 4a). The lesion was biopsied with a Tischler punch biopsy forceps under local anesthesia and the histopathology showed invasive anal cancer. A rectovaginal swab was collected for HPV genotyping. Genotyping was performed using the AmpFire platform. The sample was positive for HPV types 33, 51, and 68. She was again referred to MBH for better management. At MBH, an examination under anesthesia was performed with multiple biopsies of the cervix, posterior introitus, and perianal skin which were all positive for invasive squamous cell carcinomas. The cervical lesion was less than 1mm deep. The perianal lesion biopsy had a tumor depth of greater than 7mm. The patient then underwent a wide local excision of the perianal region, anterior and posterior vaginal walls, and a radical hysterectomy. Surgical pathology margins showed CIN3 of the cervix, VAIN3 of the anterior and VAIN1 of the posterior vagina, and micro-invasive cancer of the left perineum. The patient was referred for adjuvant chemoradiation in Douala, the economic capital of Cameroon. Due to equipment issues at this lone public radiation unit in the country, she did not receive radiation but instead received 3 weeks of daily capecitabine 500 mg at the radiation treatment center. She was later referred to a private radiation unit where she received four cycles of radiation therapy, but her condition deteriorated and she died prior to finishing treatment.
Prior to this patient’s demise, she provided consent for serial photographs and publication of her story. After her demise, her husband also provided verbal consent for her deidentified photographs to be used by our team for scientific publications.
Discussion
This case demonstrates aggressive HPV-associated invasive squamous cell carcinoma of the vulva, cervix, vagina, and anus over a time frame of two years. It has been documented that developing one type of HPV-associated cancer makes one susceptible to another HPV-associated cancer [8]. However, a case of an otherwise healthy patient, without apparent predisposing factors for HPV infection, developing four independent HPVassociated cancers in a short time period has not been reported before. Since the patient was an otherwise healthy, young female, the HPV genotypes that she was infected with were likely very virulent. Worldwide, HPV types 16 and 18 have been noted as the most virulent HPV types [2]. It is not known if the combination of these three types; 33, 51, and 68 forms a very virulent association in this population. Thus, further investigation of genotypes 33, 51, and 68 is needed in this population to uncover higher virulence. If it this true that types 33, 51, and 68 are more virulent than types 16 and 18 in this population, the only currently available HPV vaccine in this country, the Gardasil-4 (HPV quadrivalent types 6, 11, 16, and 18 vaccines, recombinant) may not be adequate to prevent HPV-associated cancers. Notably, this vaccine does not protect against any of the three types found in this case study.
Of note, the first among the four anogenital cancers to manifest was vulvar cancer. The vulvar lesion was first misdiagnosed as vulvar condyloma in several hospitals for two months before the patient got to WHP. Diagnoses of vulvar neoplasia have remained a major challenge because of its wide variability of onset. Thus, this case reinforces the recommendation that any persistent vulvar lesion such as warts that does not respond to treatment should be considered for biopsy in order to get a definitive histopathology report [11].
This case demonstrates the importance of investigating less common high-risk HPV types and associated pathologies in this population. HPV genotypes such as 33, 51, and 68 may play a significant role in invasive cancer progression in this population. Further research into different high-risk strains of HPV is necessary to better screen and vaccinate patients at risk of developing HPV-associated invasive cancers.
Declarations
Conflict of interest: The authors have no conflict of interest to disclose
Funding: Not applicable.
Acknowledgment: None.
References
- HPV and Cancer - NCI (2019). https://www.cancer.gov/aboutcancer/causes-prevention/risk/infectious-agents/hpv-and-cancer.
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021: 71: 209-49.
- Cervical cancer https://www.who.int/news-room/fact-sheets/detail/cervical-cancer.
- Sasidharanpillai S, Ravishankar N, Kamath V, Bhat PV, Bhatt P, et al. Prevalence of Human Papillomavirus (HPV) DNA among Men with Oropharyngeal and Anogenital Cancers: A Systematic Review and Meta-Analysis. Asian Pacific Journal of Cancer Prevalence. 2021; 22: 1351-1364.
- Tchouaket MCT, Fokam J, Sosso SM, Semengue ENJ, Yagai B, et al. High genotypic diversity of human papillomavirus among women in Cameroon: implications for vaccine effectiveness. IJID Regions. 2022; 5: 130-136.
- HPV Vaccination| CDC (2023). https://www.cdc.gov/vaccines/vpd/hpv/public/index.html.
- Szymonowicz KA, Chen J. Biological and clinical aspects of HPVrelated cancers. Cancer Biol Med. 2020; 17: 864-878.
- Gilbert DC, Wakeham K, Langley RE, Vale CL. Increased risk of second cancers at sites associated with HPV after a prior HPVassociated malignancy, a systematic review and meta-analysis. Br J Cancer. 2019; 120: 256-268.
- Manga S, Parham G, Nkoum B, Nulah K, Sheldon LH, et al. Cervical cancer screening in Cameroon: Interobserver agreement on the interpretation of digital cervicography results. J. Lower Genital Tract Disease. 2015.
- Zhang W, Gong X, Wu Q, Liu Y, Lao G, et al. The Clearance of High-Risk Human Papillomavirus is Sooner After Thin Loop Electrosurgical Excision Procedure (t-LEEP). Journal of Investigative Surgery. 2019; 32: 560-565.
- Manga SM, DeMarco RF, Manjuh F, Sando Z, Welty ER. Vulvar neoplasia in Cameroon, West Africa: Diagnostic challenges. Obstetrics and Gynaecology Cases-Reviews. 2018; 5: 1-6