SciBase Journals
SciBase Obstetrics and Gynecology
ISSN 2691-7785
- Article Type: Research Article
- Volume 2, Issue 1
- Received: Feb 10, 2024
- Accepted: Mar 20, 2024
- Published Online: Mar 27, 2024
Birth after Caesarean Section: A Retrospective Audit of 10 Years of State-Wide Data
Cassandra Harrison1; Ibinabo Ibiebele2; Kassam Mahomed1*
1Ipswich Hospital and University of Queensland, Ipswich, Queensland, Australia.
2University of Sydney, NSW, Australia.
*Corresponding Author: K Mahomed
Ipswich Hospital and University of Queensland, Ipswich,
Queensland, Australia.
Email: kmahomed24434@gmail.com
Abstract
Citation: Harrison C, Ibiebele I, Mahomed K. Birth after Caesarean Section: A Retrospective Audit of 10 Years of State-Wide Data. SciBase Obstet Gynecol. 2024; 2(1): 1005.
Introduction
Rates of Caesarean Section (CS) have been increasing worldwide with varying rates of [5] percent in Sub-Saharan Africa to 43 percent in Latin America and the Caribbean [1]. In Australia too rates have increased from 32 percent in 2011 to 38 percent in 20212. Attempts have been made to seek ways at slowing the rise in rates of CS but with little success [3]. Women who have had a previous CS may elect to have a Elective Repeat CS (ERCS) or have an attempt at a Vaginal Birth (VBAC) in their subsequent pregnancy. A planned VBAC, considering the woman’s individual history and needs, is viewed as a safe option for many women with a single previous lower segment caesarean section [4]. Studies have shown that a Trial of Labour (TOL) ending in a VBAC is most favourable for the mother, newborn, and the health service [5,6]. Likelihood of success rates are reported to be between 60 and 80 percent [7]. A recent meta-analysis [8] noted successful vaginal birth rates of 74.3 percent if labour was spontaneous and 60.7 percent if induced. Achieving successful VBAC has also been reported to be less expensive and more effective than undergoing an ERCS [9,10]. There has recently been an international multi-centre trial that aims to increase the proportion of women having VBAC by increasing woman-centred care and facilitating women’s empowerment in their choice of birth in three countries – Germany, Ireland and Italy [1]. An attempt at vaginal birth is also supported by various colleges across countries [4,7,12].
One of the reasons for the preference of ERCS may be a concern of a failed trial at vaginal birth resulting in an emergency CS. In one study of 29 352 women who attempted a vaginal birth after CS compared to 169 377 women without previous CS, Odds Ratio (OR) for emergency CS was 3.65 (CI: 3.26-4.08) higher when compared to women without previous CS [13]. The scibasejournals.org aim of this retrospective study however was to use a large dataset with a specific objective to report on the success and failure rate and to identify any specific predictors of a successful or an unsuccessful vaginal birth in women who are pregnant after one previous CS.
Methods
The study population included all pregnant women with a previous CS and with a singleton birth of ≥37 weeks’ gestation with cephalic presentation in a public maternity facility between 01 January 2011 and 31 December 2021. Women who had an ERCS were excluded.
Study data was retrieved from the Queensland Perinatal Data Collection (QPDC) database. The QPDC collects information on all live births and stillbirths, that occur throughout Queensland. Midwives and other medical staff complete notification forms for each birth using information obtained directly from women’s hospital charts coded by medical records staff. Completed forms and electronic extracts are validated and queries relating to missing, contradictory, or ambiguous data are directed back to the hospital or independent practitioner. Validated and confirmed data are then entered in Queensland Perinatal Data records. Diagnoses were coded using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM) and procedures using the Australian Classification of Health Interventions (ACHI).
Study variables: The outcome variable of Vaginal Birth After Caesarean (VBAC) was ascertained using a combination of the variables labour onset (no labour, induced, spontaneous) and mode of delivery (vaginal instrumental, vaginal non-instrumental, caesarean section). Births with no labour onset and caesarean section were classified as repeat elective caesarean deliveries and were excluded from the study population. Women with spontaneous or induced labour were considered to have had a trial of labour after caesarean section. Women who had spontaneous or induced labour and had a vaginal birth were considered as having a successful VBAC while those who laboured and had a caesarean section were considered as having an unsuccessful VBAC.
Maternal outcomes included uterine rupture before or during labour (ICD10AM code 0710, O711), postpartum haemorrhage, blood transfusion (ACHI code 1370601, 1370602), length of postnatal hospital stay. Neonatal outcomes included baby’s birthweight, low 5 minute Apgar score (defined as less than 7), resuscitation, hospital transfer, transient tachypnoea of newborn (P221), perinatal respiratory disorder (P20-P28 excluding P221), umbilical cord blood pH, neonatal sepsis (P36), meconium aspiration (P240), use of continuous positive airway pressure during resuscitation or treatment during the birth admission, length of stay in Special Care Nursery (SCN) or Intensive Care Nursery (ICN), and status of the baby on discharge (alive or deceased).
Other variables: Other maternal and pregnancy characteristics assessed included maternal age, Indigenous status, parity defined as the total number of previous pregnancies, any smoking during pregnancy, pre-pregnancy body mass index (<18.5, 18.5-24.9, 25-29.9, 30-39.9, ≥40 kg/m2 ), Edinburgh Postnatal Depression Scale assessment (not done, <10, 10 or more, unknown/not stated), hospital ward accommodation status (public, private), whether antenatal care was received, antenatal care provider, any current medical conditions, diabetes (ICD10AM codes: E10-E11, E13-E14, O24.0-O24.4, O24.9), hypertension (O10-O11, O13-O16), labour assistance, whether pharmacological analgesia was used, baby’s year of birth, duration from rupture of membranes to birth, duration of first and second stages of labour.
Ethics: Ethics approval was granted by West Moreton Hospital and Health Service Human Research Ethics Committee (HREC/2022/DEF/87483).
Statistical analysis: Maternal and pregnancy characteristics were compared between successful and unsuccessful VBAC groups using Chi square, T test and Mann Whitney U tests for categorical, normally, and non-normally distributed continuous data, respectively. Associations between characteristics and successful VBAC were assessed using modified Poisson regression with robust error variances. Potential predictors of successful VBAC were selected for inclusion in multivariable analysis based on statistically significant univariate association at α=0.05. Maternal and neonatal outcomes for successful and unsuccessful VBAC groups were compared using descriptive statistics.
All analyses were undertaken using SAS for Windows 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
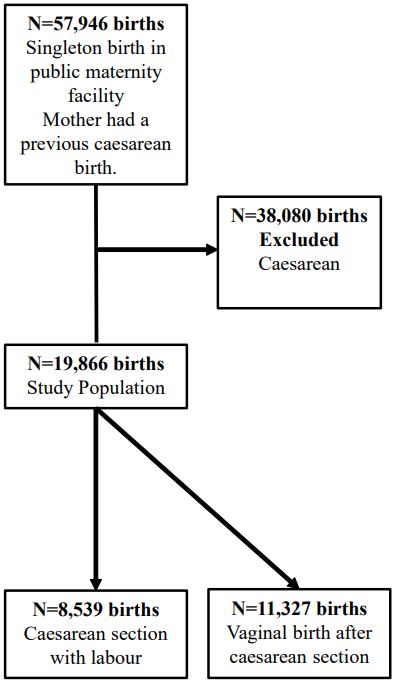
During the ten-year period from January 2011 to December 2021, there were a total of 57,946 singleton ≥37 weeks’ gestation births with cephalic presentation in public maternity facilities in Queensland to women who have had a previous caesarean birth. Of the 57,946 women, 38,080 women had an ERCS and were excluded. The study population included 19,866 women. Of these, 11,327(57%) women had a successful VBAC (Figure 1).
Table 1 demonstrates the general characteristics of the women included in the analyses based on mode of birth.
Associations between characteristics and successful VBAC were assessed using modified Poisson regression with robust error variances. Factors that increased chance of successful VBAC were increasing number of previous pregnancies, having antenatal care provided by a midwife, and labour induction or augmentation. Provision of care by a midwife was seen to increase rates of successful VBAC - both public and private midwifery models with adjusted Relative Risk (aRR) of successful VBAC 1.35 (95% CI: 1.24-1.48) and 1.15 (95% CI: 1.09-1.21) for private midwifery and public hospital midwifery care, respectively. Increasing parity increased the rate of successful VBAC with aRR 1.24 (95% CI: 1.19-1.30), 1.35 (95% CI: 1.29-1.43), and 1.42 (95% CI: 1.36-1.49) for three, four, or five previous births respectively. The use of any labour assistance including Artificial Rupture of Membranes (ARM) and/or use of oxytocin was associated with increased rate of successful VBAC with aRR 1.42 (95% CI: 1.37-1.46). Conversely, maternal age ≥35 years, maternal overweight and obesity, diabetes, hypertension, and having antenatal care provided by a medical practitioner in public hospital/clinic – were all associated with decreased risk of having a successful VBAC (Table 2).
Table 1: Characteristics of the study population by mode of birth.
| Characteristic | Vaginal birth N=11,327 | Caesarean section N=8,539 | p value |
|---|---|---|---|
| Maternal age, mean (SD) | 30.3(5.2) | 30.3(5.3) | 0.495 |
| <20 years | 98(0.9) | 103(1.2) | 0.035 |
| 20-34 years | 7651(76.4) | 6462(75.6) | |
| 35-39 years | 2149(19.0) | 1617(18.9) | |
| 40+ years | 418(3.7) | 346(4.1) | |
| missing | 11(0.1) | 11(0.1) | |
| Parity, median (IQR) | 2(1-4) | 2(1-3) | |
| 1 | 3348(29.6) | 3439(40.3) | <0.001 |
| 2 | 2923(25.8) | 2292(26.8) | |
| 3 and above | 5056(44.7) | 2808(32.9) | |
| Indigenous ethnicity, N(%) | 1254(11.1) | 935(11.0) | 0.787 |
| Any smoking, N(%) | 2096(18.5) | 1578(18.5) | 0.612 |
| Body mass index (kg/m2) | |||
| <18.5 | 485(4.3) | 346(4.1) | <0.001 |
| 18.5-24.9 | 4967(43.9) | 3394(39.8) | |
| 25.0-29.9 | 2900(25.6) | 2235(26.2) | |
| 30.0-39.9 | 2338(20.6) | 2035(23.8) | |
| 40+ | 448(4.0) | 386(4.5) | |
| Unknown | 189(1.7) | 189(1.7) | |
| Any antenatal care | 11251(99.3) | 8489(99.4) | 0.453 |
| Private specialist medical practitioner* | 203(1.8) | 166(1.9) | 0.433 |
| Private midwifery* | 336(3.0) | 153(1.8) | <0.001 |
| Public hospital midwifery* | 9288(82.0) | 6804(79.7) | <0.001 |
| Public hospital medical* | 8824(77.9) | 7016(82.2) | <0.001 |
| Private general practitioner* | 5468(48.3) | 4330(50.7) | <0.001 |
| Any medical conditions | 3786(33.4) | 3144(36.8) | <0.001 |
| Any diabetes | 1324(11.7) | 1247(14.6) | <0.001 |
| Gestational diabetes | 1280(11.3) | 1173(13.7) | <0.001 |
| Type 1 diabetes | 12(0.1) | 19(0.2) | 0.039 |
| Type 2 diabetes | 28(0.3) | 49(0.6) | <0.001 |
| Any hypertension | 335(3.0) | 323(3.8) | 0.001 |
| Pre-existing | 70(0.6) | 60(0.7) | 0.464 |
| Pregnancy induced | 181(1.6) | 155(1.8) | 0.240 |
| Pre-eclampsia/eclampsia | 99(0.9) | 114(1.3) | 0.002 |
| Any labour assistance | 5422(47.9) | 2505(29.3) | <0.001 |
| ARM | 4524(39.9) | 1960(23.0) | <0.001 |
| Oxytocin | 2472(21.8) | 1240(14.5) | <0.001 |
| Prostaglandin | 122(1.1) | 74(0.9) | 0.137 |
| Mechanical | 465(4.1) | 335(3.9) | 0.518 |
| Other | 574(5.1) | 372(4.4) | 0.020 |
*Antenatal care categories are not mutually exclusive, some women had more than one type of antenatal care provider. Percentages may sum up to more than 100% due to rounding.
Table 2: Predictors of successful VBAC.
| Characteristic | Relative Risk RR (95% CI) | Adjusted Relative Risk aRR (95% CI) |
|---|---|---|
| Maternal age | ||
| <20 years | 0.84(0.73-0.97) | 0.92 (0.75-1.14) |
| 20-24 years | 0.95(0.92-0.99) | 0.96 (0.91-1.02) |
| 25-29 years | Ref | Ref |
| 30-34 years | 0.99(0.96-1.02) | 0.97 (0.94-1.01) |
| 35-39 years | 0.98(0.95-1.02) | 0.94 (0.90-0.98) |
| 40+ years | 0.94(0.88-1.01) | 0.85 (0.78-0.93) |
| Parity | ||
| 1 | Ref | Ref |
| 2 | 1.14(1.10-1.18) | 1.13 (1.08-1.18) |
| 3 | 1.20(1.16-1.25) | 1.24 (1.19-1.30) |
| 4 | 1.32(1.27-1.38) | 1.35 (1.29-1.43) |
| 5 or more | 1.41(1.36-1.46) | 1.42 (1.36-1.49) |
| Body mass index (kg/m2) | ||
| <18.5 | 0.98(0.92-1.04) | 0.97 (0.90-1.04) |
| 18.5-24.9 | Ref | Ref |
| 25.0-29.9 | 0.95(0.92-0.98) | 0.94 (0.90-0.97) |
| 30.0-39.9 | 0.90(0.87-0.93) | 0.88 (0.85-0.92) |
| 40+ | 0.90(0.85-0.97) | 0.90 (0.83-0.97) |
| Edinburgh Postnatal Depression Scale | ||
| Not done | 1.01(0.95-1.07) | 0.97 (0.91-1.03) |
| Less than 10 | Ref | Ref |
| 10 or more | 0.92(0.88-0.97) | 0.92 (0.88-0.96) |
| Unknown/not stated | 0.88(0.66-1.16) | 0.92 (0.70-1.21) |
| Type of antenatal care provider | ||
| Private midwifery* | 1.21(1.14-1.29) | 1.35 (1.24-1.48) |
| Public hospital midwifery* | 1.07(1.03-1.10)) | 1.15 (1.09-1.21) |
| Public hospital medical practitioner* | 0.90(0.87-0.92) | 0.89 (0.85-0.92) |
| Private general practitioner* | 0.96(0.94-0.98) | 0.99 (0.96-1.02) |
| Any diabetes | 0.89(0.86-0.93) | 0.90 (0.86-0.94) |
| Any hypertension | 0.89(0.82-0.96) | 0.87 (0.80-0.95) |
| Any labour assistance | 1.38(1.35-1.42) | 1.42 (1.37-1.46) |
| Any pharmacological analgesia | 1.09(1.06-1.12) | 0.98 (0.95-1.02) |
Multivariable model adjusted for maternal age, parity, body mass index, Edinburgh perinatal depres- sion score, type of antenatal care provider, diabetes, hypertension, labour assistance, pharmacological analgesia, duration from ruptured membranes to birth, baby’s year of birth.
Discussion
The overall rate of successful VBAC was 57 percent. This rate is lower than findings from a recent meta-analysis18 that noted a success rate of 74.7% though the rates have varied from 23 to 86 percent [10,14,19-23].
Associations between characteristics and successful VBAC were assessed using modified Poisson regression with robust error variances. Factors identified increased chance of successful VBAC were increasing number of previous pregnancies, having antenatal care provided by a midwife, and labour induction or augmentation. Unfortunately, our data did not include data of previous vaginal deliveries or previous successful VBAC. Throughout the literature, the strongest predictor of successful VBAC is having a previous vaginal birth and/or previous successful VBAC [10,12,23,24]. Conducting further analysis to include this will assist in determining the outcome for our current population. It could be inferred based on our population of women undergoing labour with one previous caesarean section with parity >1, and increased success with increasing number of pregnancies. However, it is not clearly defined.
Antenatal care can be provided in several different models of care. It was demonstrated that provision of care by a midwife was seen to increase rates of successful VBAC - both public and private midwifery models. This is consistent with the “Queensland Clinical Guideline: Vaginal birth after caesarean” 25 which describes that midwifery led ‘next birth after caesarean clinic’ is effective to meet women’s information needs and address decisional conflict around VBAC [25,26]. A small prospective study carried out by Zhang and Liu [27] determined that continuing midwifery care provided during the antenatal, labour and birth, and postnatal period resulted in significantly higher rate of VBAC, reduced length of labour, and reduced Post-Partum Haemorrhage (PPH) rate. An important consideration is a woman’s experience with antenatal care, labour, and birth. An Australian survey conducted by Keedle and colleagues [28] found that women planning a VBAC benefitted from midwifery continuity of care models. Utility of models of care for women undergoing VBAC requires further attention.
Interestingly, induction or augmentation of labour was associated with successful VBAC. This is an unexpected finding as many previous studies contradict this, reporting that induction of labour was associated with unsuccessful VBAC. This included any labour assistance offered, and specifically by Artificial Rupture of Membranes (ARM), and use of oxytocin. Contrary to our findings, spontaneous labour is seen as a factor associated with successful VBAC [14,19,20,24]. Compared with spontaneous labour, induction of labour is a factor associated with unsuccessful VBAC [14,20,24]. A meta-analysis conducted by Zhang and colleagues 14 reported rates of successful VBAC as 60.7% and 74.3% with induction of labour and spontaneous labour respectively, with spontaneous labour significantly increasing rates of VBAC. Parveen and colleagues [20] determined that favourable Bishop Score (BS) was independently associated with successful VBAC. It could be postulated that induction of labour being positively associated with successful VBAC in our population may be due to local guidelines for induction of labour that recommend ARM only when the BS is greater than [6].
Maternal age ≥35 years, maternal overweight and obesity, Edinburgh Perinatal Depression Scale (EDPS) score of 10 or more, diabetes, hypertension, and having antenatal care provided by a medical practitioner in public hospital/clinic – were all associated with decreased risk of having a successful VBAC. This is consistent with reported findings in literature. Increasing maternal age was seen by Parveen and colleagues [20] as an independent factor associated with unsuccessful VBAC also shown in another stud [21]. This is consistent with a large metaanalysis conducted by Wu and colleagues [24] who found that advanced maternal age, maternal obesity, maternal diabetes, and hypertensive disorders were all factors associated with unsuccessful VBAC.
Strengths and limitations: This retrospective audit is a large study using state-wide data register - the Queensland Perinatal Data Collection - encompassing a decade of data from 2011 to 2021. Data from the register is routinely and contemporaneously collected in structured format using state-wide instructions, which ensures adequate reporting and reduced possible reporting and selection biases. The strengths of the analysis include the use of a large, heterogenous, and representative cohort. The contributing patient factors and outcomes used were welldefined.
The limitations include the lack of data relating to previous pregnancies and the index caesarean section, and birthweight as a predictor of successful VBAC. It would be useful to identify these factors as they inform counselling, with an overwhelming existing base of evidence taking these factors into account.
Conclusion
The study contributes to assisting health care providers and pregnant women wishing to have a vaginal birth with the decision-making process in understanding their chances of a successful vaginal birth. Further studies are required to explore further associations and outcomes that enable comprehensive antenatal counselling. This information could further be adapted to create a clinically useful decision-aid.
References
- Betran AP, Ye J, Moller A, Souza JP, Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health [Internet]. 2021; 6(6): 005671. Available from: https://www.ncbi.nlm.nih.gov/pmc/ doi: 10.1136/bmjgh-2021-005671.
- Australian Institute of Health and Welfare (AIHW). Australia’s mothers and babies 2021 [Internet]. Canberra (AU): Australian Institute of Health and Welfare. 2023. Available from: https://www.aihw.gov.au/reports/mothers-babies/australias-mothersbabies/contents/labour-and-birth/method-of-birth/.
- Liu S, Liston RM, Joseph KS, Heaman M, Sauve R, Kramer MS. Maternal mortality and severe morbidity associated with lowrisk planned caesarean delivery versus planned vaginal delivery at term. CMAJ {Internet]. 2007; 176(4): 455-460.
- Royal College of Obstetricians & Gynaecologists (RCOG). Birth after Previous Caesarean Birth. 2015; 45. Available from: https://www.rcog.org.uk/guidance/browse-all-guidance/greentop-guidelines/birth-after-previous-caesarean-birth-green-topguideline-no-45/.
- Fagerberg MC, Kallen K. Third-trimester prediction of successful vaginal birth after one caesarean delivery – A Swedish model. Acta Obstet Gynecol Scand [Internet]. 2020; 99(5): 660-668.
- The American Colledge of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 184: Vaginal Birth After Cesarean Delivery. Obstet Gynecol [Internet]. 2017; 130(5): 217-233.
- Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG). Best Practice Statement: Birth after previous caesarean section [Internet]. 2019. Available from: https://ranzcog.edu.au/wp-content/uploads/2022/05/Birthafter-previous-caesarean-section.pdf.
- Zhang H, Liu H, Luo S, Gu W. Oxytocin use in trial of labor after caesarean and its relationship with risk of uterine rupture in women with one previous caesarean section: a meta-analysis of observational studies. BMC Pregnancy Childbirth [Internet]. 2021; 21(11). Available from: https://bmcpregnancychildbirth.biomedcentral.com/ doi: 10.1186/s12884-020-03440-7.
- Fawsitt CG, Bourke J, Greene RA, Everard CM, Murphy A, Lutomski JE. At what price? A cost-effectiveness analysis comparing trial of labour after previous caesarean versus elective repeat caesarean delivery. PLoS One [Internet]. 2013; 8(3): e58577. Available from: https://pubmed.ncbi.nlm.nih.gov/ doi: 10.1371/journal.pone.0058577.
- Wymer KM, Shih YT, Plunkett BA. The cost-effectiveness of a trial of labor accrues with multiple subsequent vaginal deliveries. Am J Obstet Gynecol [Internet]. 2014; 211(1): 56.e1-56. 12. Available from: https://pubmed.ncbi.nlm.nih.gov/ doi: 10.1016/j.ajog.2014.01.033.
- Clarke M, Savage G, Smith V, Daly D, Devane D, Gross MM, Grylka-Baeschlin S, Healy P, Morano S, Nicoletti J, Begley C. Improving the organisation of maternal health service delivery and optimising childbirth by increasing vaginal birth after caesarean section through enhanced women-centred care (OptiBIRTH trial): study protocol for a randomised controlled trial (ISRCTN10612254). Trials [Internet]. 2015; 16(542). Available from: https://trialsjournal.biomedcentral.com/articles/ doi: 10.1186/s13063-015-1061-y.
- The American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin No. 205: Vaginal Birth After Cesarean Delivery. Obstet Gynecol [Internet]. 2019; 133(2): 110-127.
- Vaajala M, Liukkonen R, Ponkilainen V, Kekki M, Mattila VM, Kuitunen I. Ddelivery mode and fetal outcome in attempted vaginal deliveries after previous caesarean section: a nationwide registerbased cohort study in Finland. J Matern Fetal Neonatal Med [Internet]. 2023; 36(1): 2198062. Available from: https://pubmed.ncbi.nlm.nih.gov/ doi: 10.1080/14767058.2023.2198062.