SciBase Journals
SciBase Oncology
ISSN 2691-7785
- Article Type: Case Series
- Volume 1, Issue 1
- Received: Sep 19, 2023
- Accepted: Oct 20, 2023
- Published Online: Oct 27, 2023
Pathological Response and Gene Expression in Rectal Cancer Neoadjuvant Therapy
Assis Jéssica V1 *; Figueiredo Juliano A2 ; Silva Danielle J3 ; Queiroz Rafaella F4,5
1Department of Microbiology and Molecular Genetics, Michigan State University, USA.
2Adjunt Professor, Medical School, University Federal of Minas Gerais, Brazil. Coloproctologist, Hospital da Baleia, Brazil.
3Medical School Student, University Federal of Minas Gerais, Brazil.
4Diagnosis and Therapy of Infectious Diseases and Cancer, Oswaldo Cruz Foundation, Brazil.
5Faculty of Infectious Diseases, University of Georgia, USA.
*Corresponding Author: Jéssica Vieira de Assis
Department of Microbiology and Molecular Genetics, Michigan State University, USA.
Tel: +1-517-402- 6604;
Email: deassisj@msu.edu
Abstract
Rectal Adenocarcinoma (RA) represents more than 90% of rectal tumors, with high global incidence and mortality rates. Treatment includes neoadjuvant therapy, curative surgery, and postoperative adjuvant therapy. Complete Pathologic Response (CPR) signifies the absence of residual tumors and affected lymph nodes. Understanding the genetic mechanisms underlying CPR could aid in preserving organ function. Recent research identified unfavorable prognostic markers (GAPDH, CXCR4, Ki67, vimentin, tetraspanin Co029, and e-cadherin) in RA. We present two RA case reports with distinct treatment outcomes correlated with gene expression profiles. Patient one achieved CPR and remained recurrence-free, while patient two had Incomplete Pathologic Response (IPR) with lung metastases. We isolated and assessed total RNA from tumor fragments and tumor-free margins, evaluating CXCR4, GAPDH, Ki67, e-cadherin, vimentin, and TSP expression. Patient one’s tumor and tumor-free samples exhibited similar biomarker expressions, whereas patient two’s tumor fragment showed elevated expressions, particularly of CXCR4, known to promote proliferation and invasiveness. Increased expression of CXCR4, GAPDH, e-cadherin, vimentin, Ki67, and TSP was observed in rectal tumors with IPR. Our findings highlight the variable behavior of genes within the same subgroup, emphasizing the significance of exploring molecular foundations for prognostic insights.
Keywords: Rectal adenocarcinoma; Gene profiling; Pathological response; Prognosis.
Citation: Assis Jéssica V, Figueiredo Juliano A, Silva Danielle J, Queiroz Rafaella F. Pathological Response and Gene Expression in Rectal Cancer Neoadjuvant Therapy. SciBase Oncol. 2023; 1(1): 1005.
Introduction
In 2020, it was estimated that there will be more than one million new Colorectal Cancer (CRC) cases in the world, with an incidence rate of 19.5% and a mortality rate of 9% (Globocan, 2020). Brazil follows this global trend with more than 40,000 new cases annually, representing approximately 16.03% of all new tumors. In addition, 5,239 was the total number of deaths from Rectal Adenocarcinoma (RA) in the country that same year, according to data from INCA (National Cancer Institute/ Ministry of Health, 2020) [1]. It is important to consider that rectal adenocarcinoma (RA) represents >90% of rectal tumors (National Cancer Institute/Ministry of Health, 2020) [1] and presents as therapeutic methods neoadjuvant, curative surgery, and postoperative adjuvant (Wolf et al., 2020).
The evaluation of Complete Pathologic Response (CPR) is defined by the absence of residual invasive tumors and compromised lymph nodes, in surgical species (Osorio, 2012). Prognostic factors leading to recurrence and metastasis are relevant in elucidating disease outcomes (Haraldsdottir et al, 2014). National databases are considered limiting factors for the acquisition of epidemiological data since they focus mostly on primary involvement and mortality rates [2]. The main organs affected by CRC metastases are usually the liver and lung [3]. In addition, RA is also known to have some thoracic organs and the nervous system as its metastatic site [4], Leggeti B, 2010].
Local and presacral RA recurrences are most common among local recurrences and are associated with an unfavorable prognosis [5]. In contrast, anastomotic and anterior recurrences have a relatively good prognosis (Kuipers et al. 2015). Reduced tumor recurrence is associated with the performance of preoperative radiotherapy [6].
Over the past four decades, there has been a dramatic improvement in the prognosis of non-metastatic RA due to advances in staging and multidisciplinary treatment processes [7]. Subsequently, staging has been enhanced using Magnetic Resonance Imaging (MRI) and Endoscopic Rectal Ultrasonography (ERU) [8]. Furthermore, pelvic radiotherapy treatment was added and disseminated the Total Mesorectal Excision (TME) technique [9]. These factors combined contributed to reduced pelvic recurrence (4%-15%) and improved Overall Survival (OS) (69%-87%) [10].
Although relapse cases have decreased, distant metastasis remains above 25% for TNM stages II-III at 5 years [11].
In the search for more assertive therapeutic approaches, numerous trials have been conducted combining different drug families, and fractions of neoadjuvant and adjuvant radiotherapies [12]. These were aimed at reducing metastatic disease and raising Overall Survival (OS) metrics, as well as achieving a CPR so that, in this way, the chances of organ preservation in some subgroups of patients might be more tangible [13].
Personalized medicine has been widely discussed and incorporated into chronic disease management practices, such as cancer [14]. This occurs through molecular analysis of the tumor, enabling the identification, prevention, monitoring, and treatment of neoplasms in an individualized approach [15]. As a prospect, it could help in understanding CPR in patients with better prognostic profiles [16].
A recent study demonstrated a promising gene panel with impacts on the malignancy of intestinal tumors [17,18]. They found that patients who showed higher gene correlations between GAPDH, CXCR4, and E-cadherin, had worse prognoses. Numerous markers are currently studied, and this research highlights the chemokine receptor CXCR4 with an important role in the progression of intestinal tumors [19]. GAPDH, a glycolytic enzyme involved in transcript regulation and stability, acts, especially associated with CD26, in CRC metastatization [20]. The nuclear protein Ki67 indicates the proliferative capacity of tumors [21], and e-cadherin and vimentin, markers of epithelium-mesenchymal transition, are associated with cell motility and metastasis. And finally, the tetraspanin Co029 (TSP) gene favors malignant cell motility [18].
Thus, the two cases to be presented were submitted to expression profile analysis for the mentioned targets and the findings were correlated to the pathological response post-neoadjuvant
Objectives
Present two case reports where one patient had CPR and the second one had no response to neoadjuvant therapy and correlate them to the gene expression profiles of CXCR4, GAPDH, E-cadherin, tetraspanin Co029, vimentin, and Ki67.
Case presentations
The positive and negative samples from the patients involved in the study were obtained from surgical procedures at the Hospital da Baleia in Belo Horizonte, Brazil. The study was approved by the Research Ethics Committee of the Federal University of Minas Gerais under CAAE 02177612.0.3001.5091. Information on the patients, tumors, clinical management, and evolution/ outcome was obtained by analyzing and collecting data from the institution’s electronic medical records and personal documents accessed during the surgical procedure.
Unless otherwise mentioned all the chemicals used in the present study were purchased from Sigma-Aldrich (Sant-Louis, Missouri, USA).
Case 1 - Patient L.L.G., female, 72-year-old diagnosed with RA located 6 cm from the pectineal line. The tumor staging by MRI before neoadjuvant therapy was T2N2M0, clinical staging III. The patient was submitted to neoadjuvant radiotherapy and chemotherapy and had CPR with a small irregularity of the mucosa in the distal rectum (Figure 1). She was submitted to rectosigmoidectomy and histology revealed a small focus of adenocarcinoma restricted to the mucosal layer and 12 lymph nodes negative for neoplasia. The histological staging of the tumor after neoadjuvant was TisN0M0. The follow-up time after surgery for this patient is 18 months and the segment time after radiotherapy and chemotherapy is 24 months. There are no signs of recurrence or metastasis of the adenocarcinoma so far.
Case 2 - Patient A.D.A., 54-year-old male, diagnosed with RA located 6 cm from the pectineal line, The tumor staging by MRI before neoadjuvant was T3N1M0, clinical staging III. The patient was referred to neoadjuvant radiotherapy and chemotherapy and had an Incomplete Pathologic Response (IPR) with a discrete reduction in tumor dimensions. He was histologically submitted, and an ulcer-vegetative lesion was noted on the surgical specimen (Figure 2). The adenocarcinoma invaded the serous layer and there were two lymph nodes compromised out of 15 evaluated. In addition, the histological staging after neoadjuvant was T3N2M0. The segment time after surgery for this patient is 14 months, and pulmonary metastasis was noted to have appeared at 8 months postoperatively.
Gene expression evaluation
Tumor fragments and tumor-free margins of about 2 cm/2 g were collected after the excision of the surgical specimen and stored in RNA later solution (0.5M of EDTA). To obtain total RNA, extraction, and purification were performed using the TRIzol reagent (Thermo Fisher), following the manufacturer’s specifications with modifications: Samples of approximately 100 mg were macerated, and the tissue was resuspended in 1 ml of Tryzol and later precipitated in 300 µl of cold chloroform for 16 hours. After washing with 75% ethanol (MERK), total RNA was eluted in 100 µL of nuclease-free water and kept in a thermal cycler (MiniAmp Thermal Cycler, Applied Biosystems) for 30 minutes at 37°C. The isolated RNA was previously purified following the protocol of the Total RNA Purification kit (QIAGEN), and to avoid contamination of genomic DNA, the solution was treated with the DNAse I enzyme (Invitrogen). At the end of the process, 1 μl of the obtained material was used for quantification and purity analysis in NanoDrop 2000® UV-Vis Spectrophotometer (Thermo Scientific®). The remaining was stored at - 80°C until further use.
The cDNA synthesis was performed using the High-Capacity cDNA Reverse Transcription kit (Applied BiosystemsTM), following the manufacturer’s specifications with a final volume of 20 μl.
For the relative quantification assay, specific primer pairs were used for the amplification of CXCR4, GAPDH, Ki67, E-cadherin, TSP, and vimentin exons, in addition to β-actin as a normalizer, as previously described (Assis, 2020). 100 ng of cDNA was used, added 5 μl of SYBR Green PCR master mix (Applied Biosystems), 0.5 μl (400 nmol) of each primer (sense and antisense), and completed with water for a final volume of 10 μl.
Based on the relative quantification data generated using the qPCR technique, they were correlated to the tumor pathological response of the two cited patients using tudent’s t-test for parametric and nonparametric samples. Shapiro Wilk test was performed to identify the normality nature of those samples.
Results
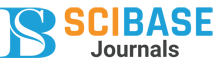
Total RNA from the samples was extracted and analyzed for gene expression by qPCR. Target expression was measured according to the endogenous gene. Despite not showing considerable statistical differences between the same marker for different individuals, patient 2 showed elevated gene expression for all the targets studied, except CXCR4 (Figure 3).
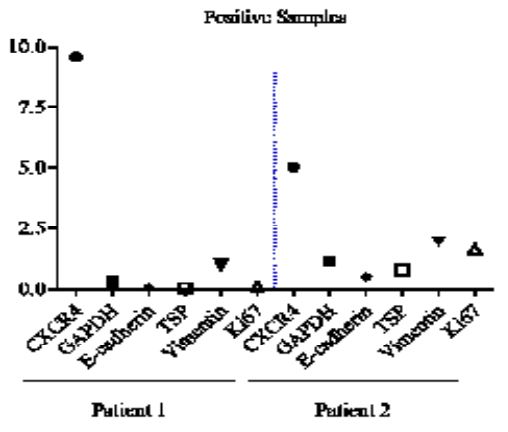
When we compare the biological groups of both patients, we notice that CXCR4 is more expressed in the tumor-positive samples than in the negative samples (Figure 4a), for both, and that GAPDH is highly expressed in the positive samples of patient 2 (Figure 4b), while patient 1 shows its upregulation in negative samples. Despite not reaching significant values, the data show different patterns for the genes studied in patients with anatomically similar tumors and different outcomes.
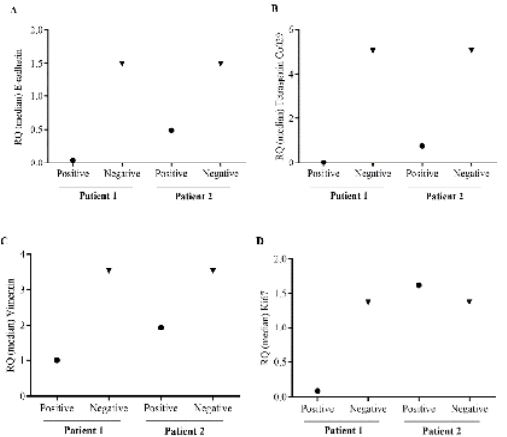
Interestingly, both patients showed higher expressions for e-cadherin, TSP, vimentin, and Ki67 in the tumor-free margins than in the tumor tissue (Figure 5a,b,c, and d), although they did not reach significant values, this data reinforces the molecular heterogeneity of tumor subgroups.
Discussion
In 2016, according to the European Society of Medical Oncology, tumors should be managed in individualized methods since studies indicate their molecular heterogeneity. To this end, the proposal of the reports was the creation of a gene panel between CXCR4, GAPDH, e-cadherin, TSP, vimentin, and Ki67 and the analysis of its correlation with the pathological response of patients. The analyses were performed using the relative qPCR technique with β-actin as the endogenous gene. For the acquisition of the DNA template for the reaction, total RNA was extracted from fresh samples.
For the comparative analyses between the positive and negative groups of each marker, a difference was observed in all targets except CXCR4, for patient 2. This profile indicates the high risk of developing metastases due they have an impact on cancer progression, especially when combined [17]. GAPDH is directly involved with tumor progression [22], which justifies its high expression level in patient 2. Its expression is associated with the risk of recurrence and lower chances of cure and survival [18]. Demonstrated that GAPDH expression is increased in colon tumors and elevated the risk of liver metastasis demonstrating its importance in the development and metastatic event [17].
Based on the Student's t-test it was not possible to establish positive correlations between the studied groups, however, CXCR4 was highly expressed in both tumor- positive samples, and GAPDH only in positive samples from patient 2. The other genes were more expressed in the tumor-free samples acquired during the surgical process and although they did not show statistical differences, they met the lack of standardization in negative sample collection which should be done carefully, to avoid collecting from areas already compromised by the pathological condition.
Finally, it is believed that these markers, associated with others, may in the future become important tools in the diagnosis and prognosis of rectal.
The study had limiting factors such as the acquisition of a small lesion mass from patient 1, only two cases to be analyzed, and the lack of guidelines for collecting tumor- free margins, reinforcing the need for further studies
Conclusion
The present study demonstrated that patients affected by RA and IPR showed higher gene expression of GAPDH, e-cadherin, TSP, vimentin, and Ki67 when compared to a patient who achieved CPR to neoadjuvant therapy. Also, IPR patients showed strong expression of CXCR4 and GAPDH in tumor-positive samples compared to disease-free margins. Thus, we conclude that those genes have the potential to be the targets of further studies regarding the mechanism determining the pathological response of patients with RA undergoing neoadjuvant therapy and organ preservation for this subgroup of patients. Additionally, that there is a need for a more in-depth analysis of techniques for excising non-tumor material from normal mucous membranes, highlighting the safety distance.
Declarations
Conflict of interest: The authors declare that they have no conflict of interest.
Financial resources: This research was supported by the Oswaldo Cruz Foundation and CAPES.
Acknowledgments: The authors sincerely acknowledge Hospital da Baleia and Universidade Federal of Minas Gerais for the present study.
References
- INCA: Instituto Nacional de Câncer. Estimativa de Câncer no Brasil, 2020.
- Yu J, Li X, Zhong C, Li D, Zhai X, et al. High-throughput proteomics integrated with gene microarray for the discovery of colorectal cancer potential biomarkers. Oncotarget. 2016; 7: 75279-75292.
- Shen X, Yue M, Meng F, Zhu J, Zhu X, et al. Microarray analysis of differentially expressed genes and linker genes associated with the molecular mechanism of colorectal cancer. Oncol Lett. 2016; 12: 3250-3258.
- Worthley D., Leggett A. Colorectal cancer: Molecular features and clinical opportunities. The Clinical Biochemist. Reviews. 2010; 31: 31-38.
- Ryan B, Zanetti K, Robles A, Schetter B, et al. Germline variation in NCF4, an innate immunity gene, is associated with an increased risk of colorectal cancer. International journal of cancer. 2014; 134: 1399-1407.
- Boland CR, Goel A. Microsatellite instability in colorectal cancer. Gastroenterology. 2010; 138: 2073-2087.e3.
- Longchamp G, Meyer J, Abbassi Z, Sleiman M, Toso C, et al. Current Surgical Strategies for the Treatment of Rectal Adenocarcinoma and the Risk of Local Recurrence. Dig Dis. 2021; 39: 325-333.
- Riihimäki M, Hemminki A, Sundquist J, Hemminki K. Patterns of metastasis in colon and rectal cancer. Sci Rep. 2016; 6: 29765.
- Delibegovic S. Introduction to Total Mesorectal Excision. Med Arch. 2017; 71: 434-438.
- Heald RJ. Rectal cancer: The surgical options. Eur J Cancer. 1995; 31A: 1189-1192.
- Erlandsson J, Holm T, Pettersson D, Berglund A, Cedemark B, et al. Optimal fractionation of preoperative radiotherapy and timing to surgery for rectal cancer (Stockholm III): A multicentre, randomized, non-blinded, phase 3, non-inferiority trial. Lancet Oncol. 2017; 18: 336-346.
- Yao Y, Xu X, Yang L, Zhu J, Wan J, et al. Patient-Derived Organoids Predict Chemoradiation Responses of Locally Advanced Rectal Cancer. Cell Stem Cell. 2020; 26: 17-26.e6
- Spring L, Fell G, Arfe A, Sharma C, Greenup R, et al. Pathologic Complete Response after Neoadjuvant Chemotherapy and Impact on Breast Cancer Recurrence and Survival: A Comprehensive Meta-analysis. Clin Cancer Res. 2020; 26: 2838-2848.
- Arredondo J, Simó V, Castañón C, Suárez MJ, Álvarez MC. Complete pathologic response after neoadjuvant chemotherapy in locally advanced colon cancer. Cir Esp (Engl Ed). 2020; 98: 168-170.
- Copur MS, Schroeder CW, Ly Q, Wedel W, Kelly JR, et al. Complete Pathologic Response to Neoadjuvant Chemoimmunotherapy and Oxaliplatin-Induced Fever Associated With IL-6 Release in a Patient With Locally Advanced Colon Cancer. Oncology (Williston Park). 2022; 36: 115-119.
- Leijssen L, Dinaux A, Amri R, Kunitake H, Bordeianou L, et al. The impact of a multi- visceral resection and adjuvant therapy in locally advanced colon cancer. J Gastrointest Surg. 2019; 23: 357-366.
- Assis J. Evaluation of gene expression and recombinant production of CXCR4 and CD26, correlated to mesenchymal epithelium transition, tumor stem cell, and cell proliferation markers in human colon and rectum tumor samples [dissertation] - Institute of Biological Sciences, Federal University of Minas Gerais. 2020.
- Coutinho L. Evaluation of the gene expression profile of human colorectal cancer laterality for a panel of markers and production of recombinant protein and antibodies to Tetraspanin CO029 [dissertation] - Faculty of Medicine, Federal University of Minas Gerais. 2020.
- Ottaiano A, Santorsola M, Del Prete P, Perri F, Scala S, et al. Prognostic Significance of CXCR4 in Colorectal Cancer: An Updated Meta-Analysis and Critical Appraisal. Cancers (Basel). 2021; 13: 3284.
- Tang Z, Yuan S, Hu Y, Zhang H, Wu W, Zeng Z, et al. Over-expression of GAPDH in human colorectal carcinoma as a preferred target of 3-bromopyruvate propyl ester. J Bioenerg Biomembr. 2012; 44: 117-25.
- Wang Y, Yang C, Bu H, Yang W, Wang L, et al. Interobserver reproducibility analysis of size-set semiautomatic counting for Ki67 assessment in breast cancer. Breast. 2020; 49: 225- 232.
- Nicholls C, Li H and Liu J. GAPDH: A common enzyme with uncommon functions. Clinical and Experimental Pharmacology and Physiology. 2012; 39: 674-679.