SciBase Journals
SciBase Oncology
ISSN 2691-7785
- Article Type: Case Report
- Volume 1, Issue 2
- Received: Oct 10, 2023
- Accepted: Nov 07, 2023
- Published Online: Nov 14, 2023
Ovarian Papillary Adenocarcinoma in a Single Young Nullipara: Challenges of Management in a Low-Income Setting
George Uchenna Eleje1,2*; Gerald Okanandu Udigwe1,2; Tobechi Kingsley Njoku2 ; Chukwuemeka Chukwubuikem Okoro2 ; Eric Chukwudi Ihekwoaba3 ; Chinedu Onwuka Ndukwe4 ; Michael Emeka Chiemeka4 ; Chukwudubem Chinagorom Onyejiaka2 ; Onyeka Chukwudalu Ekwebene5 ; Chimezuru Ogechi Duru6 ; Odili Aloysius Okoye3 ; Emeka Philip Igbodike7 ; Chigozie Geoffrey Okafor2; Nnaedozie Paul Obiegbu2 ; Divinefavour Echezona Malachy1 ; Nwabueze Chidozie Okeke2 ; Perpetua Chinedu Okolie2; Chiemezie Mac-Kingsley Agbanu2 ; Henry Chinedu Nneji2 ; Uchenna Gabriel Confidence8 ; Bernard Kachi Nwadili2 ; Chimezie Monica Ezeh9; James Egwuatu Okonkwo2 ; Ogonna Onyeka Ezenwafor2 ; Chijioke Ogomegbunam Ezeigwe1,2; Adanna Vivian Egwim2
1Department of Obstetrics and Gynecology, Nnamdi Azikiwe University, Awka, Nigeria.
2Department of Obstetrics and Gynecology, Nnamdi Azikiwe University Teaching Hospital, PMB 5025, Nnewi, Anambra State, Nigeria.
3Department of Surgery, Faculty of Medicine, Nnamdi Azikiwe University, Awka, Nigeria.
4Department of Anatomic Pathology and Forensic Medicine, Nnamdi Azikiwe University, Awka, Anambra State, Nigeria.
5Department of Epidemiology and Biostatistics, East Tennessee State University, Johnson City, Tennessee, USA.
6Department of Family Medicine, Nnamdi Azikiwe University Teaching Hospital, PMB 5025, Nnewi, Anambra State, Nigeria.
7Department of Obstetrics and Gynecology, Havana Hospital, Lagos, Nigeria.
8Changchun University of Chinese Medicine, China.
9Department of Obstetrics and Gynecology, Madonna University, Elele, Nigeria.
*Corresponding Author: George Uchenna Eleje
Department of Obstetrics and Gynecology, Nnamdi Azikiwe University, Awka, Nigeria.
Tel: +23-4806811744
Email: georgel21@yahoo.com & gu.eleje@unizik.edu.ng
Abstract
Background: Ovarian cancer is the most fatal gynecological cancer worldwide. Oftentimes, the management is challenging in low and middle-income settings. This case demonstrates for the first time a papillary serous adenocarcinoma of the ovary seen in a nulliparous young lady in our hospital, coupled with its associated management challenges.
Case presentation: She was a 26-year-old Nigerian female who presented to the gynaecology clinic with abdominal swelling of six months duration. The swelling progressively increased in size and there was associated mild pain, easy satiety and occasional nausea and vomiting. Before presentation, she had done abdominal ultrasound scan in another hospital with sonographic features suggestive of right ovarian tumor. Menarche was attained at 13 years of age and she had a regular 26-day cycle with a 5-day flow. Frozen section study came back negative for malignancy. However, the histology result showed the right ovary to be low grade papillary serous adenocarcinoma. The left ovary showed follicular cyst. The uterus, cervix, and fallopian tubes were unremarkable at histology. So far, she has been followed up for twelve months with no evidence of recurrence.
Conclusion: Papillary adenocarcinoma is a malignant tumor which usually metastasizes so early that the condition is far advanced before the patient seeks aid. It is seldomly reported with diagnostic challenges and treatment. Although it is slightly more common in parous women, the index patient was 26 years old and a nullipara, therefore showing the rarity of this malignant condition in the young. More evidence is required for management of the condition in nulliparous woman with fertility demands. Treatment can become very challenging in low-income settings.
Citation: Eleje GU, Udigwe GO, Njoku TK, Okoro CC, Ihekwoaba EC, et al. Ovarian Papillary Adenocarcinoma in a Single Young Nullipara: Challenges of Management in a Low-Income Setting. SciBase Oncol. 2023; 1(2): 1008
Introduction
Ovarian cancer is one of the three major malignant tumors in gynecology, and its incidence is third only to cervical cancer and endometrial cancer. Because of the lack of effective screening methods for ovarian cancer, 75% of patients are found to be with advanced disease at presentation [1]. Worldwide, ovarian cancer accounts for 3.4% of cancers associated with women with nearly 314000 new cases in 2020 [2]. Women with ovarian cancer often experience few or diffuse symptoms, and approximately 70% present in advanced stages-FIGO (International Federation of Gynecology and Obstetrics) stage III-IV at time of diagnosis [3]. The current standard of treatment is primary debulking surgery followed by six courses of platinum-based chemotherapy with the addition of a taxane (either paclitaxel or docetaxel) [3]. Intra-abdominal complete tumor resection is associated with a benefit in overall survival and is considered a key part in the management of epithelial ovarian cancer [4].
Ovarian cancer is the most fatal gynecological cancer worldwide, yet the fundamental mechanism of malignancy acquisition in ovarian cancer remains unknown [5]. Some factors noted to be associated with an increased risk of ovarian cancer include nulliparity, advancing age, and family history of the disease. Studies have shown that about two thirds of patients with ovarian tumors present in Stage 3 [1-3]. This may be attributed to the asymptomatic nature of the disease and the lack of effective screening methods for ovarian cancers.
At present, cancer antigen 125 (CA 125) despite its low sensitivity and limited specificity, still remains the most widely used biomarker for detection and surveillance of ovarian malignancy in the clinical setting [6]. Ultrasonography, computed tomography (CT) scan and magnetic resonance imaging (MRI) are other methods used to assess the likelihood of malignancy in women who present with adnexal masses [7]. However, none of these methods can accurately predict the malignant properties of an ovarian mass.
Ovarian cancer remains to have relatively poor prognosis particularly in low and middle-income settings [8]. It is therefore important to continually examine and report the burden of ovarian cancer to identify areas of disparities and gaps. Hence, the motive for this case report. There is disproportionate current and future burden of ovarian cancer in countries with lower Human Development Index (HDI) levels such as Nigeria, calling for global action to reduce the burden and inequality of ovarian cancer in access to quality cancer care and treatment [8]. We herein report the achievement of ‘successful’ treatment of a rare case of a papillary serous adenocarcinoma in a young nulliparous lady, without any evidence of post treatment recurrence. This case demonstrates for the first time a papillary serous adenocarcinoma of the ovary seen in a nulliparous young lady in our hospital.
Case presentation
She was a 26-year-old Nigerian female who presented to the gynecology clinic with abdominal swelling of six months duration. The swelling progressively increased in size and there was associated mild pain, easy satiety and occasional nausea and vomiting. She presented with an abdominal ultrasound scan with features suggestive of right ovarian tumour. Menarche was attained at 13 years of age and she had a regular 26-day cycle with a 5-day flow.
A general physical examination revealed that she had welldeveloped secondary sexual characteristics. Systemic examination of the abdomen revealed a distended abdomen that moves with respiration with no tenderness, however an abdominopelvic mass of 18 weeks size and ascites demonstrable by fluid thrill was noted. Other systems were largely normal
Vaginal examination revealed normal vulva/vagina, healthylooking nulliparous os with a firm cervix. Right adnexa mass of about 18 weeks size was noted with no adnexal tenderness or cervical excitation tenderness.
Basic laboratory investigation done was largely normal. The CA 125 level was 19.5 units/ml. Chest x-ray showed normal findings with no features suggestive of metastasis. Computed tomography of the abdomen done revealed a complex midline abdominopelvic mass highly suggestive of ovarian malignancy, with associated significant ascites. Following this, informed consent was obtained in preparation for surgery. She was also counselled on need for cryopreservation but she declined. Consult was sent to the anesthetist and the pathologists were invited for the frozen section.
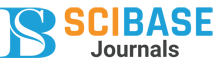
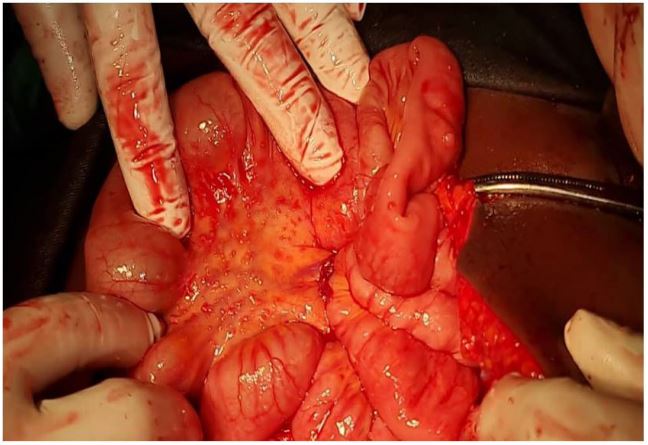
During surgery, the following intra-operative findings were made: Adhesion involving the omentum and the bladder; serous ascitic fluid of about 2.5L; right ovarian mass measuring about 20 cm X 12 cm with weight of about 2 kg. Metastatic deposits were noted on the gut, surface of the liver, omentum, mesentery and anterior abdominal wall (Stage 3B, Figure 1). The gross image of the specimen is shown in Figure 2. The left ovary, left tube and the uterus were apparently healthy-looking. The frozen section specimen was collected by the pathologist. After waiting for more than an hour for the result of the frozen section, total abdominal hysterectomy, bilateral salpingooophorectomy and infra-colic omentectomy was done based on clinical judgement. The patient’s intraoperative bleeding was 250 mL and the postoperative course was uneventful.
Post-operatively, she was managed with intravenous antibiotics (ceftriaxone and metronidazole), intravenous fluids (5% dextrose water alternated with normal saline), and analgesics (pentazocine and rectal diclofenac). After 48 hours, all her intravenous drugs were converted to oral medications. She was placed on haematinics. Patient had an uneventful recovery and was discharged on the 8th day post-surgery after a counselling on the intra-operative findings, the surgery done, the need for histology and subsequent management.
The intraoperative findings and post-operative histological diagnosis were not consistent with the frozen section diagnosis. Results of the frozen section revealed overall features that are negative for malignancy. Sections from the tissue labelled fallopian tube showed fibrous tissue. No tubal epithelium. No neoplastic cell seen. Sections from the ovary showed normal ovarian follicles and ovarian stroma. Sections from the omental tissue showed fat aggregates with surrounding fibrocollagenous stroma and marked inflammatory infiltrates. Overall features are negative for malignancy.
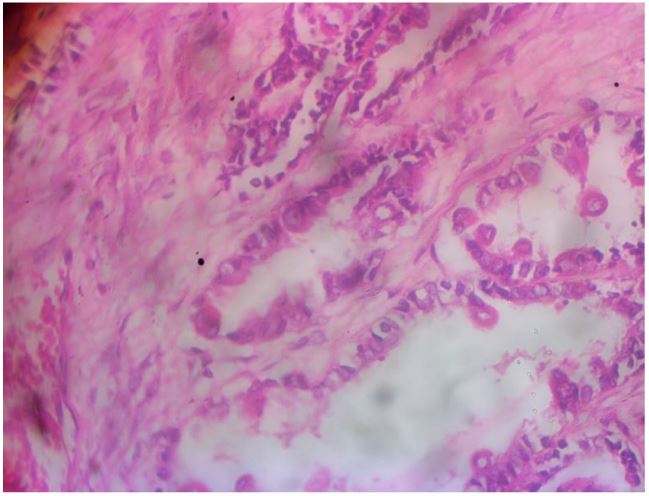
Meanwhile, the histology done on the salpingo-oophorectomy specimen showed findings suggestive of low grade papillary serous adenocarcinoma. Sections of the right ovary shows an invasive tumor composed of glands disposed in papillary fronds. The lining cells have round hyperchromatic nuclei, prominent nucleoli with moderate eosinophilic cytoplasm. The stroma was cellular and fibrocollageneous. Mitosis was noted including abnormal forms. No psammoma bodies or necrosis were noted. The overall features were those of low grade papillary serous adenocarcinoma. The photomicrograph is shown in Figure 3. Sections of the left ovary showed follicle cysts and ovarian stroma. The left ovary was not involved by the tumor. Section of the cervix, uterus and fallopian tubes were unremarkable and not involved by the tumor. Patient was counselled on the findings and worked up for chemotherapy using carboplatin with area under the curve of 5 and paclitaxel at a dose of 75 mg/m2 . Postoperatively, she received six courses of chemotherapy which were well tolerated. Follow-up visit 12 months after surgery showed an apparently healthy young lady without any evidence of recurrence. The patient gave her informed consent for the publication of this case report.
Discussion
Papillary adenocarcinoma is a malignant tumor of the ovary which usually metastasizes so early that the condition is far advanced before the patient seeks aid. The average age at which it occurs is approximately fifty years [7]. It is slightly more common in parous than in nulliparous women. However, our index patient was 26 years and a nullipara therefore showing the rarity of this malignant condition in the young. Previous reported cases in the literature were cases in the middle-aged or aged population. For example, Kim et al. reported a rare case of ovarian mesonephric-like adenocarcinoma involving the fimbria and mimicking serous tubal intraepithelial carcinoma [9]. It was a case of a 47-year-old woman that presented with a 4.4 cm left ovarian mass with histology of the ovary showing papillary and solid architecture, severe nuclear pleomorphism, and increased mitotic activity [9].
Although a clear etiologic factor responsible for the development of ovarian cancer has not been identified, the risk of the disease is inversely proportional to the number of lifetime ovulations. Thus, factors associated with suppression of ovulation, such as increasing numbers of full-term pregnancies, longer duration of lactation and oral contraceptive use are associated with a decrease in ovarian cancer. Factors associated with greater lifetime ovulation and/or greater lifetime estrogen exposure such as nulliparity, early age of menarche, and use of hormone replacement therapy increase risk which was all obtained in the index patient and therefore contributory risk factors [9]. Furthermore, inflammatory conditions such as endometriosis appear to increase risk of ovarian cancer, whereas tubal ligation and hysterectomy reduce risk. Ovarian cancer is more common in industrialized countries, and available epidemiologic data suggest that environmental factors may contribute to development of the cancer, although this remains uncertain [8,9]. Cigarette smoking appears to increase the risk of some subtypes though not contributory in the index case [7,9].
The diagnosis was suspected by gynecological examination, ultrasound imaging, and computed tomography imaging (CT) and confirmed histologically post-surgery. In terms of treatment, surgery and chemotherapy are the mainstay of treatment to eliminate as many cancer cells as possible. The surgical methods are total hysterectomy, bilateral fallopian tube-ovarian resection, and comprehensive stage exploration to completely remove the tumor and avoid tumor rupture as much as possible [10]. However, the choice between laparotomy and minimally invasive surgery for ovarian cancer is currently controversial [10]. In one recent study that analysed the surgical and oncological outcomes of three different surgical approaches in a large series of ovarian cancer patients, revealed that no significant difference was found in overall survival and disease-free survival among the three groups (open, laparoscopic, and robotic). The minimally invasive approach showed lower rate of complications than the laparotomic approach [11]. In another study, aimed at comparing the outcomes of advanced ovarian cancer patients who had minimally invasive surgery with outcomes of advanced ovarian cancer patients who had laparotomy for interval cytoreduction after neoadjuvant chemotherapy, it was concluded that minimally invasive surgery is feasible and effective for interval cytoreduction after neoadjuvant chemotherapy in advanced ovarian cancer patients. Minimally invasive surgery was associated with less blood loss, lower transfusion rate, and shorter length of hospital stay with no difference in patient outcomes [12]. Our patient was treated with total abdominal hysterectomy, bilateral ovariectomy and infra-colic omentectomy to reduce the tumor mass. She also received adjuvant chemotherapy and has been followed up at regular intervals.
Although frozen section was done for the patient, the delay in getting the result necessitated the use of clinical judgement intra-operatively to carry out the surgical resection. Frozen section is an intraoperative diagnostic procedure performed on tissue, which is frozen and sectioned with cryostat, stained and viewed under the microscope by a pathologist who has been informed preoperatively [13]. The result of the frozen section assists the surgeons to decide on further management especially with regards to the extent of surgery since it provides a preliminary diagnosis. Rakhshan et al. in 2009 studied the use of frozen section in the diagnosis of ovarian masses and reported an overall accuracy as high as 95.7% [13]. The sensitivity of frozen section diagnosis for benign, borderline and malignant lesions was 99%,60%, and 92%, respectively; whereas the sensitivities of gross examination and clinical data in distinguishing benign from non-benign lesions were 93 and 70%, respectively [13]. We could not rely on the result of the frozen section, apart from the fact that the result came quite late. In one recent Cochrane review, the largest discordance is within the reporting of frozen section borderline tumours [14]. Investigation into factors leading to discordance within centres and standardisation of criteria for reporting borderline tumours may help improve accuracy [14].
Metastatic ovarian cancer is difficult to cure. The main treatment has remained surgery and post-surgical adjuvant chemotherapy. Our index patient had a staging laparotomy with hysterectomy invariably at this age will stop her monthly menstrual flow. This will also affect her fertility potentials. Young patients who wish to retain fertility can undergo a unilateral fallopian tube and oophorectomy for stage I and low-risk ovarian tumors (early stage, low-grade aggressive tumors, and low malignant potential ovarian tumors). In the late or infiltrating phase, cytoreductive surgery is the main method and is also the initial treatment recommendation for patients with stages II, III, and IV disease. However, the uterus and ovaries were removed in our patient, thereby pushing her into surgical menopause. We gave the patient an explanation about late complications after the surgery. She agreed to receive the surgical procedures in favour of tumor control despite her young age reproductive wishes. Unfortunately, her future reproductive potential is in jeopardy leaving her with few options such as surrogacy with oocyte donation and adoption.
Our patient received six courses of adjuvant chemotherapy and post chemotherapy condition has been satisfactory. She has been on follow-up visits for 12 months without any experience of recurrence. Our post-chemotherapy findings corroborate those of the previous data regarding the clinical presentation of ovarian adenocarcinoma. For instance, Koh et al. investigated the clinicopathological, immunohistochemical, and genetic features of ovarian mesonephric-like adenocarcinoma. Four patients with stage IC-II tumor underwent post-operative adjuvant chemotherapy [15]. Three of the four patients whose follow-up information was available did not experience recurrence. In contrast, the remaining patient with stage IA tumor who did not receive any adjuvant treatment developed multiple metastatic recurrences at post-operative 13 months [15].
Additionally, Wu et al. has described mixed cell ovarian adenocarcinoma which is a malignant gynecological tumor consisting of serous, mucous, and papillary tumor cells [10]. A total of 2,818 patients diagnosed with mixed cell ovarian adenocarcinoma were identified, and the 5-year survival rate was 62%. After propensity score matching for age, grade, and stage, the 5-year survival rate was 69.7% for ovarian serous cystadenocarcinoma and 62.9% for ovarian papillary serous cystadenocarcinoma. These results mean that serous adenocarcinoma had the best prognosis of the three pathologic types of ovarian carcinoma (p<0.001), with no significant difference between papillary serous cystadenocarcinoma and mixed cell ovarian adenocarcinoma [10]. These various histotypes have been previously reported in a Nigerian multi-centre study [16].
Unlike in our case, few patients after cytoreductive surgery retain child-bearing potential due to the high rate of hysterectomy and oophorectomy at time of surgery [17]. Efforts towards enhanced preoperative counselling for cryopreservation, increased oocyte and embryo cryopreservation, and assessing the safety of conserving reproductive organs at the time of surgery are desirable [17].
Conclusion
Papillary adenocarcinoma is a malignant tumor which usually metastasizes so early that the condition is far advanced before the patient seeks aid. It is seldomly reported with diagnostic challenges and treatment. Although it is slightly more common in parous women, the index patient was 26 years old and a nullipara, therefore showing the rarity of this malignant condition in the young. More evidence is required before recommendations of management of papillary serous adenocarcinoma in a nulliparous woman with fertility demands. Treatment can become very challenging in low-income settings. Our successful observations should encourage the multi-disciplinary team of care.
Declarations
Acknowledgments: The authors thank the histopathology department of NAUTH, Nnewi, Nigeria.
Disclosure: The authors declare that they have no conflicts of interest in this work.
Ethics: An informed consent was obtained from the patient to allow the reporting of this case as well as the use of her intraoperative picture.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions: GUE, GOU, TKN and CCO1 conceived, supervised the study and performed the surgery; ECI, CON, OAO, CGO, and CCO2 analyzed data; OCE, COD, NPO, DEM, NCO, JIM, JEO, UGC, PCO, CMA, HCN, AVE and OOE wrote the manuscript; EPI and GUE made manuscript revisions. All authors reviewed the results and approved of the final version of the manuscript.
Ethics approval and consent to participate: Not applicable.
Consent for publication: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests: The authors declare that they have no competing interests.
Financial support/sponsorship: The authors declared that this study has received no financial support.
References
- Berek JS, Renz M, Kehoe S, Kumar L, Friedlander M. Cancer of the ovary, fallopian tube, and peritoneum: 2021 update. Int J Gynaecol Obstet. 2021; 155(1): 61-85. doi: 10.1002/ijgo.13878.
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021; 71(3): -249. doi: 10.3322/caac.21660.
- Sørensen SM, Høgdall C, Mosgaard BJ, Dalgaard MIR, Jensen MP, Fuglsang K, et al. Residual tumor and primary debulking surgery vs interval debulking surgery in stage IV epithelial ovarian cancer. Acta Obstet Gynecol Scand. 2022;1 01(3): 334-343. doi: 10.1111/aogs.14319.
- Du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer. 2009; 115(6): 1234-44. doi: 10.1002/cncr.24149.
- Chen G, Yan Y, Qiu X, Ye C, Jiang X, Song S, et al. miR-93-5p suppresses ovarian cancer malignancy and negatively regulate CCND2 by binding to its 3’UTR region. Discov Oncol. 2022; 13(1): 15. doi: 10.1007/s12672-022-00478-1.
- Sölétormos G, Duffy MJ, Othman Abu Hassan S, Verheijen RH, Tholander B, Bast RC Jr, et al. Clinical Use of Cancer Biomarkers in Epithelial Ovarian Cancer: Updated Guidelines From the European Group on Tumor Markers. Int J Gynecol Cancer. 2016; 26(1): 43-51. doi: 10.1097/IGC.0000000000000586.
- Fischerova D, Burgetova A. Imaging techniques for the evaluation of ovarian cancer. Best Pract Res Clin Obstet Gynaecol. 2014; 28(5):697-720. doi: 10.1016/j.bpobgyn.2014.04.006.
- Cabasag CJ, Fagan PJ, Ferlay J, Vignat J, Laversanne M, Liu L, et al. Ovarian cancer today and tomorrow: A global assessment by world region and Human Development Index using GLOBOCAN 2020. Int J Cancer. 2022. doi: 10.1002/ijc.34002.
- Kim H, Bae GE, Jung YY, Kim HS. Ovarian Mesonephric-like Adenocarcinoma With Multifocal Microscopic Involvement of the Fimbrial Surface: Potential for Misdiagnosis of Tubal Intraepithelial Metastasis as Serous Tubal Intraepithelial Carcinoma Associated With Ovarian High-grade Serous Carcinoma. In Vivo. 2021; 35(6): 3613-3622. doi: 10.21873/invivo.12667.
- Wu H, Jiang S, Zhong P, Li W, Zhang S. Development and identification of a prognostic nomogram model for patients with mixed cell adenocarcinoma of the ovary. J Ovarian Res. 2021; 14(1): 137. doi: 10.1186/s13048-021-00896-9.
- Cianci S, Capozzi VA, Rosati A, Rumolo V, Corrado G, Uccella S, et al. Different Surgical Approaches for Early-Stage Ovarian Cancer Staging. A Large Monocentric Experience. Front Med (Lausanne). 2022; 9: 880681. doi: 10.3389/fmed.2022.880681.
- Brown J, Drury L, Crane EK, Anderson WE, Tait DL, Higgins RV, et al. When Less Is More: Minimally Invasive Surgery Compared with Laparotomy for Interval Debulking After Neoadjuvant Chemotherapy in Women with Advanced Ovarian Cancer. J Minim Invasive Gynecol. 2019; 26(5): 902-909. doi: 10.1016/j.jmig.2018.09.765.
- Rakhshan A, Zham H, Kazempour M. Accuracy of frozen section diagnosis in ovarian masses: experience at a tertiary oncology center. Arch Gynecol Obstet. 2009; 280(2): 223-8. doi: 10.1007/s00404-008-0899-6.
- Ratnavelu ND, Brown AP, Mallett S, Scholten RJ, Patel A, Founta C, Galaal K, Cross P, Naik R. Intraoperative frozen section analysis for the diagnosis of earlystage ovarian cancer in suspicious pelvic masses. Cochrane Database Syst Rev. 2016; 3(3): CD010360. doi: 10.1002/14651858.CD010360.pub2.
- Koh HH, Park E, Kim HS. Mesonephric-like Adenocarcinoma of the Ovary: Clinicopathological and Molecular Characteristics. Diagnostics (Basel). 2022; 12(2): 326. doi: 10.3390/diagnostics12020326.
- George SHL, Omotoso A, Pinto A, Mustapha A, Sanchez-Covarrubias AP, Umar UA, et al. An Assessment of Ovarian Cancer Histotypes Across the African Diaspora. Front Oncol. 2021; 11: 732443. doi: 10.3389/fonc.2021.732443.
- Violette C, Kim T, Shandley L, Lee R, Staley C, Winer J, et al. Fertility after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: A call to action. J Surg Oncol. 2021; 123(4): 1045-1049. doi: 10.1002/jso.26387.