SciBase Journals
SciBase Surgery
ISSN 2691-7785
- Article Type: Case Report
- Volume 1, Issue 1
- Received: Sep 27, 2023
- Accepted: Oct 31, 2023
- Published Online: Nov 07, 2023
Recovery of Achilles Tendon Rupture with Bone Marrow Aspirate Matrix: A Case Report
Rodrigo Vicente1 ; Gabriel Silva Santos1* ; Madhan Jeyaraman2-5; Lucas Furtado da Fonseca1,6; Daniel Shuiti Igarashi Ueno7 ; Mauricio D’arc Palmieri8 ; Leonardo Pires6 ; Petrick Seidy Neves Sato9 ; José Fábio Lana10,11,12,13
1Brazilian Institute of Regenerative Medicine (BIRM), Indaiatuba, SP, Brazil.
2Department of Orthopaedics, Faculty of Medicine, Sri Lalithambigai Medical College and Hospital, Dr MGR Educational and Research Institute, Chennai 600095, Tamil Nadu, India.
3Department of Biotechnology, School of Engineering and Technology, Sharda University, Greater Noida 201310, Uttar Pradesh, India.
4South Texas Orthopaedic Research Institute (STORI Inc.), Laredo, Texas 78045, USA.
5Indian Stem Cell Study Group (ISCSG) Association, Lucknow 226010, Uttar Pradesh, India.
6Federal University of São Paulo (UNIFESP), São Paulo, SP, Brazil.
7Medicine School of Marilia (FAMEMA), Marília, SP, Brazil.
8Nove de Julho Hospital, São Paulo, SP, Brazil.
9Ultra Sports Science, São Paulo, SP, Brazil.
10Medical School, Max Planck University Center (UniMAX), Indaiatuba, SP 13343-060, Brazil.
11Department of Orthopedics, Brazilian Institute of Regenerative Medicine (BIRM), Indaiatuba, SP 13334-170, Brazil.
12Regenerative Medicine, Orthoregen International Course, Indaiatuba, SP 13334-170, Brazil.
13Clinical Research, Anna Vitória Lana Institute (IAVL), Indaiatuba, SP 13334-170, Brazil.
*Corresponding Author: Gabriel Silva Santos
Brazilian Institute of Regenerative Medicine (BIRM), 1386 Presidente Kennedy Avenue, Cidade Nova I, Indaiatuba, SP, Brazil.
Tel: +5519989283863;
Email: gabriel1_silva@hotmail.com
Abstract
Achilles Tendon (AT) rupture is a common debilitating condition associated with ankle and foot overuse injuries. This disorder can often prove to be challenging since tendons are poorly vascularized structures that rely on synovial fluid diffusion in order to obtain nutrients. The deficit in strength due to AT rupture may increase the risk of additional injuries and complications. Surgical interventions are usually the first choice of treatment, but problems may still persist during follow-up. Conversely, the administration of orthobiologics has revealed high success rates in several procedures associated with regenerative medicine. Popular autologous alternatives, such as Bone Marrow Aspirate (BMA), are often utilized in clinical settings. Our patient received only one session of “BMA matrix” injections, displaying satisfactory healing based on functional assessments, Magnetic Resonance Imaging (MRI) results, and pain scores. The patient was able to return to sports with no complaints and MRI scans obtained during follow-up revealed clear signs of AT restoration. Here, we discuss a safe and effective administration of an autologous BMA product as a feasible alternative for the enhanced healing of a musculoskeletal tissue injury.
Keywords: Case report; Achilles tendon; Orthobiologics; Bone marrow aspirate; Regenerative medicine.
Citation: Vicente R, Santos GS, Jeyaraman M, Lucas Furtado dF, Daniel Shuiti IU, et al. Recovery of Achilles Tendon Rupture with Bone Marrow Aspirate Matrix: A Case Report. SciBase Surg. 2023; 1(1): 1003.
Introduction
AT ruptures are one of the most common lower limb injuries [1]. This disorder can affect elite and amateur athletes who perform vigorous repetitive maneuvers, including jumping and running [2]. AT injuries in general can sometimes be complicated to treat since tendons are poorly vascularized structures which obtain nutrition via synovial fluid diffusion [3]. A healing tendon forms a fibrous scar tissue, therefore making it biomechanically weaker in comparison to healthy tissue [4]. This fragility can predispose the patient to further injury and complications. AT rupture treatment with orthobiologics envisages restoration of the original tissue properties and reduce the risk of additional injuries [5].
There is still controversy regarding the most effective treatment alternative for acute Achilles tendon rupture [6]. Conservative treatment of AT rupture usually requires cast immobilization for approximately 6 weeks. The ankle is placed in a cast in plantar flexion for the first 4 weeks and then in neutral position for the remaining period [6]. There is great concern surrounding the fact whether conservative treatment of a ruptured tendon is feasible without direct contact with surrounding structures. Conservative strategies are linked to higher rates of rerupture in comparison to surgical procedures [7]. Nevertheless, it is important to note that delayed healing can result in calf weakness. Incomplete healing, in turn, may predispose patients to the risk of reruptures [6].
Progressive research in regenerative medicine has allowed orthopedic surgeons to appreciate and report enhanced biological effects of orthobiologics. These products are obtained from the body itself and carry the potential to ameliorate tissue repair processes in orthopedic conditions [8]. The most popular examples found in the medical literature are Hyaluronic Acid (HA), Platelet-Rich Plasma (PRP) and bone marrow products, such as Bone Marrow Aspirate (BMA) [9].
The attractive feature about BMA is that it is clinically feasible since it imparts significant regenerative attributes, especially in terms of musculoskeletal recovery [8]. BMA carries Hematopoietic Stem Cells (HSCs) and Mesenchymal Stem Cells (MSCs) [9]. These cells are highly praised for their capacity to secrete a plethora of bioactive molecules. These, in turn, allow them to dictate the biological alterations in the local tissue microenvironment due to paracrine and autocrine signaling [9]. Additionally, they can perform self-renewal and differentiation into specific mature cell lineages, further contributing to the healing cascade [9].
In order to achieve healing, the damaged tissue requires a few steps, such as progenitor cell recruitment and differentiation, fibroblast proliferation, collagen production, angiogenesis, and physiological loading [10]. Orthobiologic administration for the treatment of painful musculoskeletal disorders, such as AT injuries, still requires additional studies and there is much to be discussed. Here, we report the application of the “BMA matrix” [9] as an alternative for the healing of AT rupture.
Materials and methods
A 52-year-old female amateur street runner and yoga instructor was suffering from pain in the right Achilles tendon since 2017. She had previously been submitted to physical therapy and conservative treatments, including infiltration with corticosteroids but no clinical improvement was achieved. The injury worsened in 2020 with restriction of daily activities due to claudication.
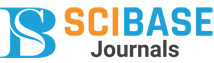
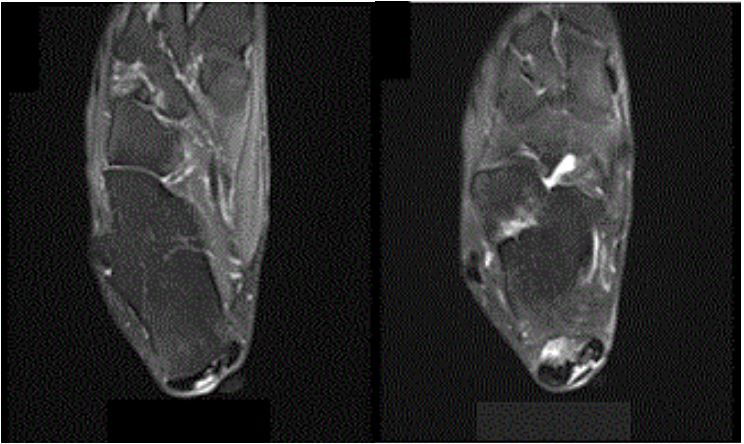
Degeneration of the body of the Achilles tendon with granuloma and paratendinous cyst was identified via MRI scans (Figures 1a and 1b). The patient underwent open surgery (Figure 1c) for tenoplasty of the body of the tendon and resection of the paratendinous cyst. In the first 3 months after the operation she had a satisfactory clinical evolution with well tolerated progressive load and total load without the use of orthopedic boots. At 4 months postoperatively, during the physiotherapy session, she presented sudden posterior pain in the calcaneus when performing strength exercise for triceps surae.
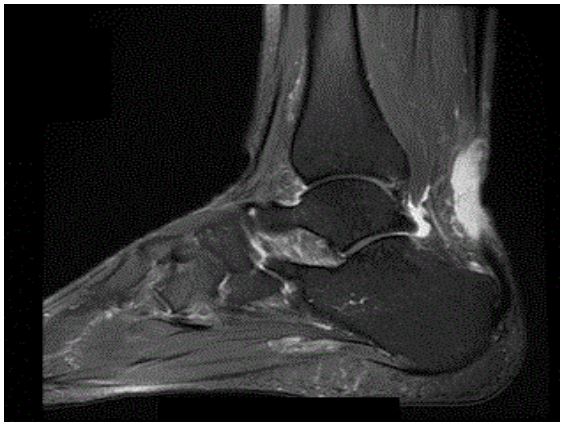
A new imaging exam showed partial rupture of the Achilles tendon at its calcaneal insertion, affecting 40% of the transverse section (Figures 2a and 2b). Given the previous condition of tendinopathy in the body of the Achilles tendon and moderate insertional partial tear, surgical treatment was chosen for arthroscopic transfer of the long flexor of the hallux to the posterosuperior wall of the calcaneus. In the area of the Achilles tear, we decided to consider an approach with ultrasoundguided “BMA matrix” infiltration into the lesion focus.
Surgical procedure
Patient was positioned in ventral decubitus under spinal anesthesia and venous sedation via posterolateral and posteromedial access for posterior ankle arthroscopy identification of the flexor hallucis longus tendon in the posterior talar groove. Tenotomy of the long flexor of the hallux and repair of the proximal stump with fiberwire under fluoroscopic aid, and reaming of the calcaneus on the upper wall in its most posterior and medial portion were performed. We also performed transposition of the proximal stump of the flexor hallucis into the reamed canal and fixation with 1 biotenodesis screw with tensioning with the foot maintained in a slight physiological equinus of 5°.
BMA matrix preparation
Identification of the posterior superior iliac spine was done using ultrasound. Local anesthesia of the bone plate and periosteum was achieved with 10 ml of ropivacaine. 15 ml of BMA were collected in 3 syringes of 10 ml (5 ml per syringe), with rapid suction of the aspirate according to the Hernigou technique [11]. The final 5 ml was transferred and kept in a 5 ml syringe. BMA was mixed with 2 ampoules of medium molecular weight hyaluronic acid (osteonil plus) in a three-way stopcock in order to form the “BMA matrix” [9]. 8 ml of the final solution were injected in the area of insertional rupture with ultrasound guidance. The remaining 7 ml were distributed in the retroachilles bursa and insertion point of the flexor tendon of the transposed hallux. The skin of the arthroscopy portals was sutured, a compressive dressing with gauze and bandage was applied, and a plastered splint was placed in a physiological equine. Postoperatively, the patient kept the splint for 1 week until medical reassessment. Use of orthopedic boots was maintained up to the third week after the procedure. Progressive loading was achieved for additional 6 weeks and full loading at 9 weeks post operatively.
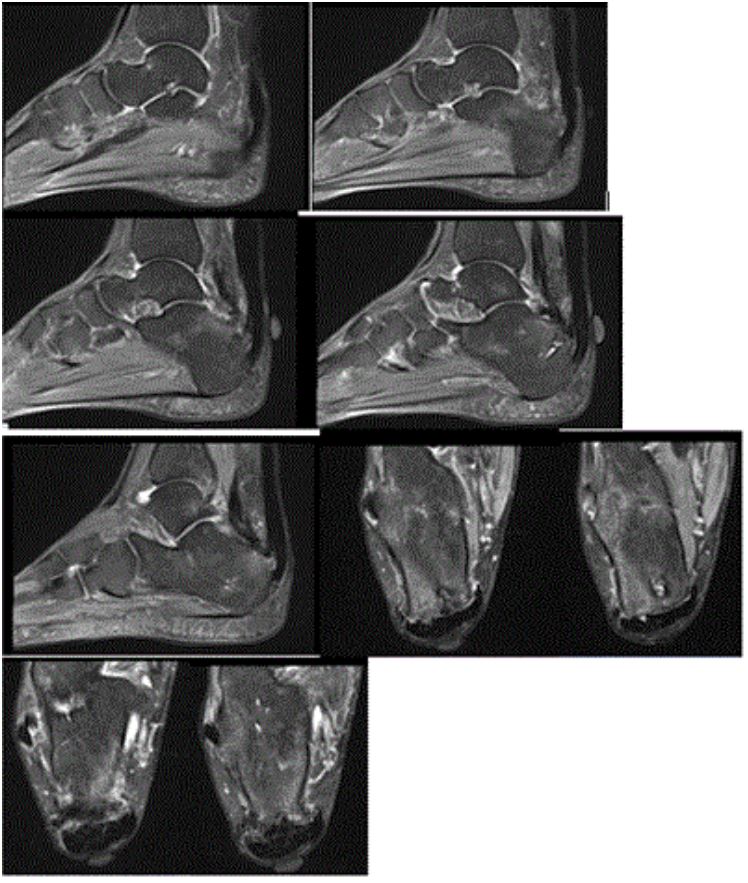
Results
Before treatment, the patient had a score of 9 on the Visual Analogue Scale (VAS). MRI scans taken before the interventional procedures reveal an increase in the extensive partial rupture of the Achilles tendon close to the distal insertion. It extends from the topography of the posterior calcaneal spur to just above the posterosuperior margin of the calcaneus, for approximately 3.1 cm in the longitudinal direction and 1.5 cm in the lateral direction. It affected more than 50% of the tendinous area with greater irregularity and change in the signal of the centromedial fibers. This was also associated with an inflammatory response with subcutaneous edema and liquid distension of the deep retrocalcaneal bursa.
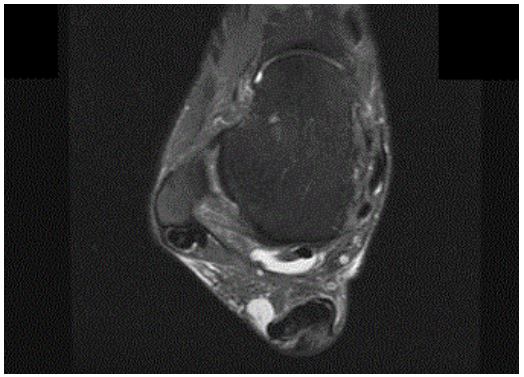
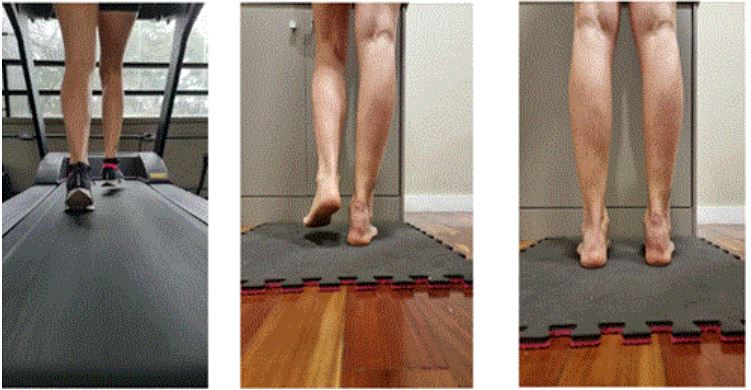
After the procedure the patient felt much better, scoring a 1 on the VAS test and presented no physical limitations for sports; she was able to run a half-marathon in just 6 months postoperatively (Figures 3 & 4).
Discussion
AT ruptures are common lower limb injuries that frequently occur in athletes who engage in repetitive activities such as jumping and running [1,2]. Treating these injuries can be challenging because tendons have limited blood supply and receive nourishment through synovial fluid diffusion [3]. During the healing process, the tendon forms a fibrous scar tissue, which is weaker and less resilient than healthy tissue [4]. This weakness increases the risk of further injuries and complications. Orthobiologic treatments aim to restore the original properties of the tendon and reduce the risk of additional injuries [5].
The most effective treatment approach for acute Achilles tendon rupture is still a topic of controversy [6]. Conservative treatment typically involves immobilizing the ankle in a cast for approximately 6 weeks, initially in a plantar flexed position and then in a neutral position for the remaining period [6]. There are concerns about the feasibility of conservative treatment without direct contact with surrounding structures. Conservative strategies have been associated with higher rates of rerupture compared to surgical procedures [7]. However, it’s important to consider that delayed healing can lead to calf weakness, and incomplete healing increases the risk of reruptures [6].
Soft tissue injuries in healthy patients generally don’t require prolonged healing times, though the duration can vary based on the severity of the injury and individual factors [12]. In the case of our physically patient who was already 52 years old at the time of the accident, a speedy recovery was observed with just one session of BMA matrix injections, as indicated by MRI scans and questionnaire data. Traditional management strategies for AT ruptures often involve interventions like open surgery, but these procedures may not always suffice and there are risks. Among the complications associated with AT ruptures, re-rupture is considered the most significant complication following treatment [13]. Healing of damaged tendons involves several important steps, including the recruitment and differentiation of progenitor cells, proliferation of fibroblasts, production of collagen, angiogenesis, and physiological loading [10]. Therefore, alternative approaches such as the administration of orthobiologics may be convenient for accelerated tissue repair. Bone marrow-derived products, in particular, have shown promise as a regenerative medicine tool not only for musculoskeletal tissues but also for other organ systems in various diseases [14-16].
One potential alternative for healing AT ruptures is the application of the “BMA matrix” as described by Lana et al. in 2021 [9]. This approach utilizes bone marrow aspirate and hyaluronic acid to enhance the crosslinking of fibrin fibers in order to create a rich biological matrix that reinforces healing of the Achilles tendon. The fibrin matrix serves as a biological scaffold and a reservoir of cytokines and growth factors, which in turn enhances the activity of MSCs present in BMA. As mentioned earlier, MSCs possess the ability to undergo self-renewal and differentiate into various types of mesodermal lineage cells, including bone, fat, cartilage, muscle, meniscus, and tendon [17]. Moreover, MSCs play a crucial role in modulating the local tissue microenvironment through autocrine and paracrine effects.
These cells offer significant advantages as they are not known to elicit aggressive immune responses and can be readily isolated, enabling allogeneic transplantation if needed [9]. However, the effectiveness of these therapies is largely dependent on the MSCs’ ability to home and engraft into the target tissues. MSCs have a relatively short lifespan and are eventually engulfed by monocytes, leading to the stimulation of T-regulatory cell production. This series of events significantly contributes to overall clinical improvement [9].
Following tissue injury, local cells release cytokines to attract MSCs to the site. Upon recruitment, MSCs respond by producing molecular factors such as Vasculoendothelial Growth Factor (VEGF), Transforming Growth Factor Beta (TGF-β), Stromal-Derived Factor 1 (SDF-1), and Stem Cell Factor (SCF), among others. These growth factors enable MSCs to exert further control over the healing process by inhibiting fibrosis and apoptosis, dampening excessive inflammation, and promoting cell proliferation and differentiation through paracrine and autocrine signaling [9]. This is extremely important in order to dampen the chronic inflammatory process associated with tendon rupture and provide it enough time to regenerate properly in a more favorable microenvironment.
Interleukin-1 receptor antagonist (IL-1Ra) plays a significant role in the healing process. This potent cytokine present in the bone marrow, acts as a competitive antagonist by binding to IL-1β and IL-1α receptors, thereby inhibiting IL-1-induced catabolic reactions and inflammatory stress [18,9]. This may partially explain the significant improvements in pain observed in our patient. IL-1Ra can slow down the degradation of the extracellular matrix, as IL-1β is known to induce the expression of matrix metalloproteinase 3, tumor necrosis factor alpha, and prostaglandin E2. IL-1Ra is also associated with preventing chondrocyte apoptosis and inhibiting collagen deposition [9]. In fact, an animal study [18] showed that IL-1Ra administration reverses the changes associated with established tendinopathy. In the context of tendon injuries, the beneficial effects mediated by IL-1Ra are crucial for restoring tissue homeostasis and facilitating proper fiber reconstruction. Other recent investigations in human models revealed that the application of both BMA and BMAC (bone marrow aspirate concentrate) products promote safe and effective tendon healing, eliminating pain and restoring function [19,20,21].
Conclusion
In this case report, our patient responded positively to treatment without experiencing any serious adverse effects. While there are several studies evaluating bone marrow-derived products for tendon pathologies in general, there is a notable lack of clinical investigations specifically focusing on the use of BMA products for AT ruptures. However, considering the success of BMA in regenerative medicine for lower limb conditions, we were confident in employing orthobiologic administration, and the results met all of our expectations. The use of the “BMA matrix” led to significant improvements in pain, functional outcomes, and visible signs of soft tissue healing after one treatment session. Remarkable effects were observed within 6 months post treatment, as the patient was able to return to all activites without pain or any sort of physical impediment. Further research is still warranted in order to fully comprehend the mechanisms underlying this technique.
Declarations
Ethics approval and consent to participate: Consent was obtained from the patient for participation in the medical procedure
Consent for publication: Consent was obtained from the patient for the use of CT scans in this manuscript.
Availability of data and material: N/A.
Competing interests: Authors declare no conflict of interest.
Funding: N/A.
Authors’ contributions: All authors contributed equally to the production of this manuscript.
References
- Li HY, Hua YH. Achilles Tendinopathy: Current Concepts about the Basic Science and Clinical Treatments. BioMed Research International. 2016; 2016.
- Waldecker U, Hofmann G, Drewitz S. Epidemiologic investigation of 1394 feet: Coincidence of hindfoot malalignment and Achilles tendon disorders. Foot and Ankle Surgery. 2012; 18: 119-23.
- Fenwick SA, Hazleman BL, Riley GP. The vasculature and its role in the damaged and healing tendon. Arthritis Research. 2002; 4: 252-60.
- Yang G, Rothrauff BB, Tuan RS. Tendon and ligament regeneration and repair: Clinical relevance and developmental paradigm. Birth Defects Research Part C-Embryo Today: Reviews. 2013; 99: 203-22.
- Dhillon M, Behera P, Patel S, Shetty V. Orthobiologics and platelet rich plasma. Indian Journal of Orthopaedics. 2014.
- Park SH, Lee HS, Young KW, Seo SG. Treatment of Acute Achilles Tendon Rupture. Clin Orthop Surg. 2020; 12: 1-8.
- Khan RJK, Fick D, Keogh A, Crawford J, Brammar T, et al. Treatment of acute achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2005; 87: 2202-10.
- Santos Duarte Lana JF, Furtado da Fonseca L, Mosaner T, Tieppo CE, Marques Azzini GO, et al. Bone marrow aspirate clot: A feasible orthobiologic. Journal of Clinical Orthopaedics and Trauma. 2020.
- Lana JF, da Fonseca LF, Azzini G, Santos G, Braga M, et al. Bone marrow aspirate matrix: A convenient ally in regenerative medicine. International Journal of Molecular Sciences. 2021.
- Yuan T, Zhang CQ, Wang JHC. Augmenting tendon and ligament repair with platelet-rich plasma (PRP). Muscles, Ligaments and Tendons Journal. 2013.
- Hernigou P, Trousselier M, Roubineau F, Bouthors C, Chevallier N, et al. Stem Cell Therapy for the Treatment of Hip Osteonecrosis: A 30-Year Review of Progress. Clin Orthop Surg. 2016; 8: 1.
- Guo S, DiPietro LA. Factors Affecting Wound Healing. J Dent Res. 2010; 89: 219-29.
- Hanada M, Takahashi M, Matsuyama Y. Open re-rupture of the Achilles tendon after surgical treatment. Clin Pract. 2011; 1: e134.
- Bozdag-Turan I, Goekmen Turan R, Ludovicy S, Akin I, Kische S, et al. Intra coronary freshly isolated bone marrow cells transplantation improve cardiac function in patients with ischemic heart disease. BMC Res Notes. 2012; 5: 195.
- Chahla J, Alland JA, Verma NN. Bone Marrow Aspirate Concentrate for Orthopaedic Use. Orthop Nurs. 2018; 37: 379-81.
- Vahidy FS, Haque ME, Rahbar MH, Zhu H, Rowan P, et al. Intravenous Bone Marrow Mononuclear Cells for Acute Ischemic Stroke: Safety, Feasibility, and Effect Size from a Phase I Clinical Trial. Stem Cells. 2019; 37: 1481-91.
- Purita J, Lana JFSD, Kolber M, Rodrigues BL, Mosaner T, et al. Bone marrow-derived products: A classification proposal-bone marrow aspirate, bone marrow aspirate concentrate or hybrid? WJSC. 2020; 12: 241-50.
- Eskildsen SM, Berkoff DJ, Kallianos SA, Weinhold PS. The use of an IL1-Receptor Antagonist to Reverse the Changes Associated with Established Tendinopathy in a Rat Model. Scand J Med Sci Sports. 2019; 29: 82-8.
- Farina KA, Kandah BA, Sowers NM, Moore GA. Bone Marrow Aspirate Concentrate Injection Of The Achilles Tendon In A Competitive Distance Runner. Journal of Musculoskeletal Research. 2021; 24.
- Imam MA, Holton J, Horriat S, Negida AS, Grubhofer F, et al. A systematic review of the concept and clinical applications of bone marrow aspirate concentrate in tendon pathology. SICOT-J. 2017; 3: 58.
- Thueakthong W, de Cesar Netto C, Garnjanagoonchorn A, Day J, Friedman G, et al. Outcomes of iliac crest bone marrow aspirate injection for the treatment of recalcitrant Achilles tendinopathy. International Orthopaedics. 2021