SciBase Journals
SciBase Surgery
ISSN 2996-590X
- Article Type: Research Article
- Volume 1, Issue 1
- Received: Oct 09, 2023
- Accepted: Nov 29, 2023
- Published Online: Dec 06, 2023
Chronic Pain After Complete Extraperitoneal Inguinal Hernia Repair: A Randomised Controlled Trial Comparing Glue and Absorbable Tackers
Hassan A Saad1*; Azza Baz2; Mohamed Riad1; Mohamed E Eraky1; Ahmed El-Taher1; Mohamed I Farid1 ; Khaled Sharaf1
1Surgical Department, Faculty of Medicine, Zagazig University, Zagazig City, Sharquia, Egypt.
2Surgical Department, Alahrar Teaching Hospital, Zagazig City, Sharquia, Egypt.
*Corresponding Author: Hassan A Saad
Surgical Department, Faculty of Medicine, Zagazig University, Zagazig City, Sharquia, Egypt
Tel: (+20) 01221025689;
Email: ebramos2010@yahoo.com
Abstract
Abstract: After having an inguinal hernia fixed, approximately 20% of people endure chronic pain. The underlying mechanism most likely involves sensory nerve damage and abnormal recovery, which may be influenced by the materials employed to secure the mesh. The major purpose of this study was to look at the impact of glue and absorbable tackers on the occurrence of residual discomfort after surgery in people who had totally extraperitoneal inguinal hernia repair (TEP).
Methods: Patients having (TEP) inguinal hernia surgery were randomly assigned to either absorbable tackers (hold STRAP Johnson & Johnson) or glue to hold the mesh (LIQUIBAND secure 8 Neopharm) in a single-blind clinical trial. A validated 4-point verbal-rank scale with the categories “none,” “mild,” “moderate,” and “severe” was used to score pain at one week, one month, six months, and a year after surgery. Chronic painful hernial location that persists for more than 6 months.
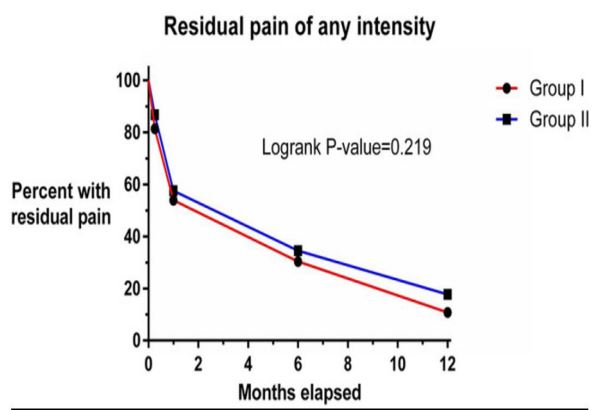
Results: 218 patients were subjected to analyses. The groups differed just slightly in terms of age, gender, and hernia side. After 6 months, 31.7%(66/208) and 13%(29/208) of those who reported chronic pain of any intensity continued to do so, respectively. There were no different changes between the both categories in post surgery pain with the two methods, only patients suffering with significant discomfort, glue-using was still less uncomfortable than tacker-based fixation (log-rank p = 0.025). After a year, four symptomatic recurrence hernias were detected in individuals whose mesh was patched with absorbable tackers.
Conclusions: Patients who had mesh put into place for TEP inguinal hernia surgery reported less pain.
Citation: Saad HA, Baz A, Riad M, Eraky ME, El-Taher A, et al. Chronic Pain After Complete Extraperitoneal Inguinal Hernia Repair: A Randomised Controlled Trial Comparing Glue and Absorbable Tackers. SciBase Surg. 2023; 1(1): 1005.
Introduction
The commonest elective surgical procedure in open and laparscopic is inguinal henia and its post surgery problem, the pain presenting 16-62% of postoperative problems [1]. The adoption of endoscopic methods has significantly reduced the prevalence of groyne discomfort, although up to 20% of those who have had laparoscopic therapy may still have persistent pain [2]. Despite the fact that postoperative groyne pain is always mild in nature but the problems in long period pain that can significantly impair usual activities [1,3].
Although convoluted and difficult to classify in multiple cases, the underlying aetiology of postoperative groyne discomfort is not well known. Because more cases experience post surgery painless area, loss of sensation or numbness, it indicates that other variables besides nerve damage sustained during surgery are at work [1]. Another widely proposed rationale for the use of mesh is a chronic foreign body inflammatory reaction [2]. Postoperative discomfort may be increased if the prolein mesh well fixed to the abdomen with glue or tackers, as is done [4]. Tackers put deeper into tissue, such as the muscles of the abdomen wall or the pubic bone, are thought to have a higher-up of hypersensitivity reaction and possibility of postsurgical problems of persistent agony in comparison to procedures of wellfixed mesh utilization.
A recent reseaches found the absorble tacer and glue have the same low rate of recurrency and postsurgery agonic sensation [5]. As a result, we decided to conduct a randomised trial to compare these two approaches.
The primary goal of this study was to examine the effects of absorbable tackers and glue on postoperative chronic pain after mesh fixation in TEP inguinal hernia surgery.
Methods design
We conducted a single-blind, randomised clinical trial in which we compared the use of absorbable tack staples versus glue to anchor mesh in TEP hernia repair patients.
Participants selection
Our cases admitted from surgery from 2020-2023, elective clinic and must be between the ages of 18 and 80.
1. Patients with large co-morbid that interfer with pain measurment or anaethesia or any measurements were excluded from the trial, as did those who had prior groyne surgery.
2. Pregnant women.
3. Patients with large inguinoscrotal, recurrent hernia, obstructed, strangulated, and inflammed hernias were also excluded irreducible or incarcerated hernias.
Randomization: Randomization was made using sealed envelopes, which were opened in the operating room just before mesh fixation.
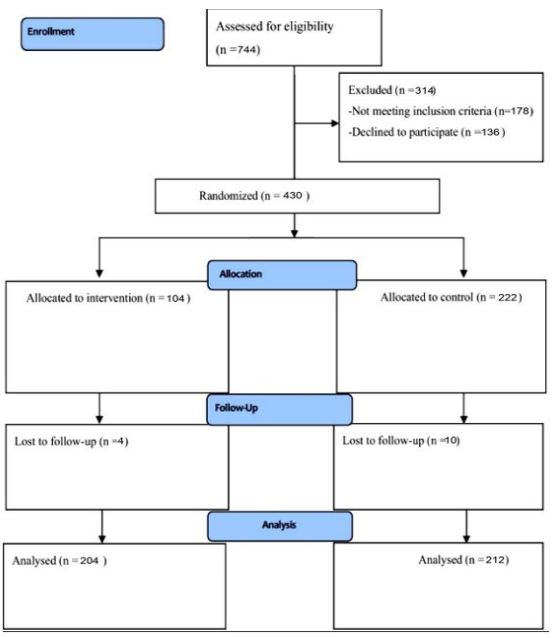
Intervention: Enrollment flowchart
Randomization: Figure 1: Participant registration flowchart, Randomization, Before mesh fixation, the sealed envelopes used for randomization and explored in the theature.
Intervention
Patients in Group II had absorbed tacers (SECURE STRAP, Johnson & Johnson, USA) attached to the tissue, whereas patients in Group I had mesh attached with adhesive (LIQUIBAND FIX 8, Liquiband, Advanced Medical Solutions, UK). The treatment done under general anaesthesia by five arranging surgeons, TEP repair is the standard operating, All patients received 2 g of intravenous cefazolin and prophylactic antibiotics prior to surgery. Three trocars were typically utilised during TEP inguinal hernia surgery, and the 30 degree came had an 11 mm umblical opening, two 5 mm trocker above the pubis, 4 cm and 8 cm respectively. This study did not use pre-peritoneal balloons to dissect the pre-peritoneal cavity. A knitted polypropylene mesh of the appropriate size used (Bard 3Dmax, BD, USA). At the same fixation area, the mesh was attached lateral to the transverse fascia, we used 4 tacker or four glue maximally in every individuals (medially, somewhat above the pubis, into iliopubic track, and medially, into the fascia transversalis) it is one day surgery, so patients discharged with standard postoperative care instructions.
Results
Patients examination, one week later at outpatient clinic. A cellphone connection was used 1,3,6 month, post surgery. All participants examination about pain (type, level and site) and activity (Quality of life) using a 4-point verbal-rank scale [7]. While moderate pain interfered with daily activities and was rarely treated with analgesics, severe pain was described as incapacitating, happening frequently, or interfering with activities, and mild pain as intermittent pain or discomfort with self-recovery and the need for analgesia. Daily exercise included both athletic and physical activities such as jogging, bag lifting, and strolling. Chronic pain was defined as suffering that lasted longer than three months after surgery [7].
Statistics for analysis
For the statistical analysis, GraphPad Prism (version 6.00 for Windows, GraphPad Software, La Jolla, California, USA) and R (version 4.1.0, R Foundation for Statistical Computing) were used. Descriptive data for continuous and categorical factors were shown as mean (standard deviation) or number (%). Correlation analysis using independent t-tests and 2-tests to compare the two groups, were used for continuous and categorical variables, respectively. Time-to-event curves were established for each of the groups reporting residual pain. The log-rank test was used to assess the differences in the time-to-event curves. Means, standard deviations, and percentages were rounded to the nearest decimal place, whereas p-values were rounded to the nearest thousandth place.
Table 1: Baseline characteristics.
| Group I | Group II | P-value | ||
|---|---|---|---|---|
| Age | Mean (SD) | 54.5 (16.3) | 54.5 (16.0) | 0.972 |
| Gender | Male | 192 (94.1%) | 198 (93.4%) | 1.000 |
| Female | 12 (5.9%) | 14 (6.6%) | ||
| Sides | Unilateral | 68 (33.3%) | 72 (34.3%) | 1.000 |
| Bilateral | 136 (66.7%) | 140 (65.7%) | ||
| Hernia type | Direct | 86 (25.1%) | 98 (27.8%) | 0.34 |
| Indirect | 240 (70.2%) | 226 (64.2%) | ||
| Pantaloon | 16 (4.7%) | 28 (8.0%) | ||
| Large hernia | 20 (5.8%) | 26 (7.4%) | 0.67 | |
| Lipoma | 62 (18.1%) | 72 (20.5%) | 0.59 |
Recruitment details
During the study period, 744 people were screened who had laparoscopic TEP inguinal hernia surgery at the zagazig university hospital them did not match the inclusion criteria, and 136 patients rejected to participate. The 430 participants (398 males and 32 women) were randomly assigned to one of two study groups. Fouty patients were left out because they were not followed up with at the end of the research. Figure 1 summarises the study flowchart from eligibility determination to final analysis. COVID-19 pandemic constraints prohibited 34 patients from visiting the outpatient clinic for an evaluation one year after surgery. The phone pain interviews with these patients were viewed as a minor procedural breach.
Default characteristics
In the study, 436 people received 692 laparoscopic TEP repairs, including 276 with bilateral hernias and 140 with unilateral hernias. There were no noticeable differences in the distribution of age and gender among the groups (Table 1). One year after surgery, 34 patients (16 from group 1 and 18 from group 2) were unable to visit the outpatient clinic for a physical examination.
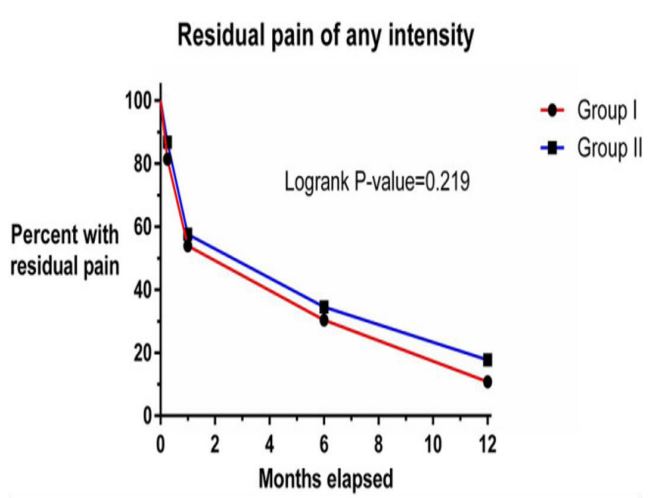
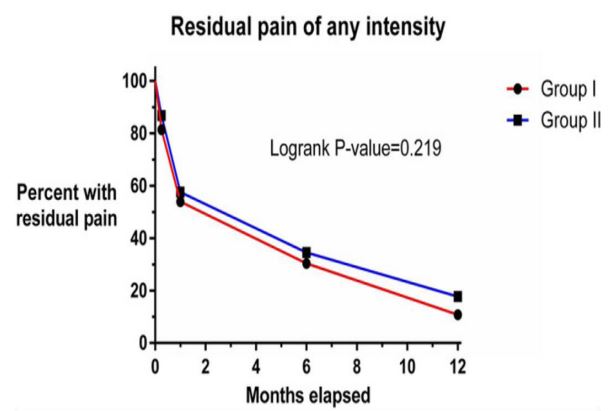
After one month, 54.8% (228/416) of patients who underwent surgery reported persistent pain of any degree, 31.7% (132/416) six months later, and 13% (58/416) after a year (Figure 2). According to methods of mesh fixation our individual subdivided into two categories, there were no variations in the degrees of moderate to severe agony (Figure 3). Only 1% of patients suffered severe pain one year after surgery, compared to 11% one week later. There were fewer patients feeling severe discomfort at each time point when mesh fixation was performed using glue rather than tacer technique (log-rank p = 0.025) (Figure 4).
Recurrences of hernias and postoperative complications
Two cases group 2 was rehopitalized due to a inguinal swelling due to bleeding, and four patients from group 1 suffering retention of urine. There were no wound-related issues discovered.
Twenty recurrent unilateral hernias were found in 2 patient in the glue fixation group and 18 patients in the tacer group (p = 0.02). The 4 recurrent cases were female and elderly (70 8). 16 individuals had indirect hernias at the time of the initial operation. On 18 people, the first both sides operation in the same time for indirect hernia was performed. Regarding group 2 we found 8 patients suffering from recurrent herniation by symptoms, all of symptomatic recurrent cases discovered through the first 4 months but an asymptomatic recurrent inguinal hernia was discovered by physical exam during first six months.
Discussion
The major goal of this study was to see if the kind of mesh fixation had an effect on chronic pain. There were no variations in the degree of chronic pain between persons who had their glue procedure and those who had their tacker fixation. Patients who had mesh glued to them with adhesive were less likely to develop severe chronic pain, according to our findings. These data show that mesh fixation with adhesive would be preferred for TEP hernia surgery patients. Laparoscopic TEP is now the standard treatment for inguinal hernia repair. The majority RCTs had a restricted number of participants or used a combination of TEP and transabdominal preperitoneal repair. Lindstrem et al.’s great research on the Swedish national hernia concluded after TEP repaire ther is improving of agony but the rate of recurrency still high [8].
Adjustment of the size of the mesh is very important to cover the exact defect and prevent the mesk from migration. Several authors proposed that the preperitoneal space be adequately placed with no anchoring to prevent future tissue injury and minimise the prevalence of persistent pain [9]. In a randomised controlled experiment (RCT), Moreno-Egea et al. found no differencs between mesh fixation by tacer or glue or sutures and without any fixation in the rate of persistent pain [10].
Chronic inguinal pain affects 1-2% of patients who undergo laparoscopic hernial procedure [4]. Techapongsatorn et al. chose glue as the best mesh fixation method in a recent review of 11 RCTs, finding no statistically significant differences between them.
Chih-Chin Yu et al. [11] evaluated data from a single institution on 583 participants after TEP technique and discovered that patients with mechanical fixation had a higher rate of acute groyne pain than those with adhesive. The incidence of persistent groyne pain, however, were comparable among groups.
Following laparoscopic surgery, 1 to 13% of patients have recurrent inguinal hernia [4,12]. Because many studies did not consistently track their subjects over time and only actively investigated them if they presented repeated hernia symptoms, these figures are likely to underestimate the true recurrence rate. One year after surgery, attending surgeons in our study evaluation 34 patients, in reality, only 8 patients experienced a symptomatic recurrence. 12 patients had no symptoms discovered by exam and confirmed by ultrasonography. These cases blindley discoved during first year follow up. Recurrencey of hernias were far more common in patients with absorbable tracker-secured mesh than in patients with glue-secured mesh in our study, indicating that glue may have some extra benefits. The reason for this disparity is unknown, but both procedures the mesh was hold in the pre-peritoneal area allowing better time for healing by fibrosis. When employing tacers, it is important to fix the mesh in the pubic bone to be secured effectivelly. All the operators were professional in using tacer so, any misuse must be excluded. The work has various constraints were affecting the results. Lack of connection with the participants because far hospitat distance or negligence or another exam in near clinic, all leading to diminish in our observation. A larger sample size in the study could have resulted in more accurate results for a visual representation of surgical complications and pain assessment. We solely looked at pain and how it interfered with daily activities in this study. We did not evaluate any additional quality of life outcomes.
Conclusions
The using of the glue instead of absorbable tackers during laparoscopic TEP hernia surgery minimises severe Inguinal pain and hernia recurrence.
Declarations
Acknowledgments: Not applicable.
Declaration and ethical clearance: Ethical clearance was obtained from Zagagic University, Faculty of Medicine, Institutional Health Research Ethics (IHRERC), and written informed consent was obtained from the Review IHRERC under No. (ethical protocol number ZU-IRB#99902792023). Written informed consent was obtained from all patients and obtained from the Zagazig University Hospital, all database done in accordance with the Declaration of Helsinki.
Consent for publication: Not applicable.
Availability of data and materials: A database is available to the corresponding author. This database is available for review and request. All authors have agreed and shared the database.
Competing interests: The authors declare that they have no competing interests or financial disclosures.
References
- Mui WL, Ng CS, Fung TM, et al. Prophylactic ilioinguinal neurectomy in open inguinal hernia repair: a double-blind randomized controlled trial. Ann Surg. 2006; 244(1): 27-33. doi: 10.1097/01.sla.0000217691.81562.7e.
- Öberg S, Andresen K, Rosenberg J. Decreasing prevalence of chronic pain after laparoscopic groin hernia repair: a nationwide cross-sectional questionnaire study. Surg Today. 2018; 48(8): 796-803. doi: 10.1007/s00595-018-1664-5.
- Aasvang E, Kehlet H. Surgical management of chronic pain after inguinal hernia repair. Br J Surg. 2005; 92(7): 795-801. doi: 10.1002/bjs.5103.
- Alabi A, Haladu N, Scott NW, et al. Mesh fixation techniques for inguinal hernia repair: an overview of systematic reviews of randomized controlled trials. Hernia. 2021; 2021: 1-15. [PMC free article]
- Techapongsatorn S, Tansawet A, Kasetsermwiriya W, et al. Mesh fixation technique in totally extraperitoneal inguinal hernia repair - a network meta-analysis. Surgeon. 2019; 17(4): 215-224. doi: 10.1016/j.surge.2018.09.002.
- Claus C, Furtado M, Malcher F, Cavazzola LT, Felix E. Ten golden rules for a safe MIS inguinal hernia repair using a new anatomical concept as a guide. Surg endos. 2020; 34: 1458-1464. doi: 10.1007/s00464-020-07449-z.
- Classification of chronic pain Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986; 3: 1-226.
- Lundström K-J, Holmberg H, Montgomery A, Nordin P. Patientreported rates of chronic pain and recurrence after groin hernia repair. Br J Surg. 2018; 105(1): 106-112. doi: 10.1002/bjs.10652.
- Taylor C, Layani L, Liew V, Ghusn M, Crampton N, White S. Laparoscopic inguinal hernia repair without mesh fixation, early results of a large randomised clinical trial. Surg Endosc. 2008; 22: 757-762. doi: 10.1007/s00464-007-9510-7.
- Moreno-Egea A, Torralba Martinez JA, Morales CG, Aguayo Albasini JL. Randomized clinical trial of fixation vs nonfixation of mesh in TEP inguinal hernioplasty. Arch Surg. 2004; 139: 1376-1379. doi: 10.1001/archsurg.139.12.1376.
- Yu CC, Chen YT, Huang CS, Chueh SC, Lo CW, Tsai YC. Ching-Shui Huang A comprehensive study comparing tack and glue mesh fixation in laparoscopic total extraperitoneal repair for adult groin hernias. Surg Endosc. 2020; 34: 4486-4493. doi: 10.1007/s00464-019-07234-7.
- Siddaiah-Subramanya M, Ashrafi D, Memon B, Memon MA. Causes of recurrence in laparoscopic inguinal hernia repair. Hernia. 2018; 22: 975-986. doi: 10.1007/s10029-018-1817-x.